Scientists from Japan and Australia have teamed up to develop and validate a blood test for Alzheimer’s disease, with the potential to massively ramp up the pace of Alzheimer’s disease drug trials.
The blood test measures a specific peptide in the blood to inform scientists, with 90 per cent accuracy, if a patient has the very earliest stages of Alzheimer’s disease.
Blood samples from patients in a large study from the Japanese National Center for Geriatrics and Gerontology (NCGG) were initially analysed to identify the relevant peptides. Those indicating brain beta-amyloid burden were then tested against patient samples from the Australian Imaging, Biomarker and Lifestyle Study of Aging (AIBL), to validate the results.
Professor Katsuhiko Yanagisawa, Director-general of Research Institute at NCGG, says: “Our study demonstrates the high accuracy, reliability and reproducibility of this blood test, as it was successfully validated in two independent large datasets from Japan and Australia.”
Dr Koichi Tanaka at Shimadzu Corporation was instrumental in developing the initial blood testing procedure. Professor Tanaka won the Nobel prize in Chemistry in 2002 for the technique. “From a tiny blood sample, our method can measure several amyloid-related proteins, even though their concentration is extremely low. We found that the ratio of these proteins was an accurate surrogate for brain amyloid burden.”
One of the essential hallmarks of Alzheimer’s disease is buildup of abnormal peptide in the brain, called beta-amyloid. The process starts silently about 30 years before outward signs of dementia, like memory loss or cognitive decline, have begun.
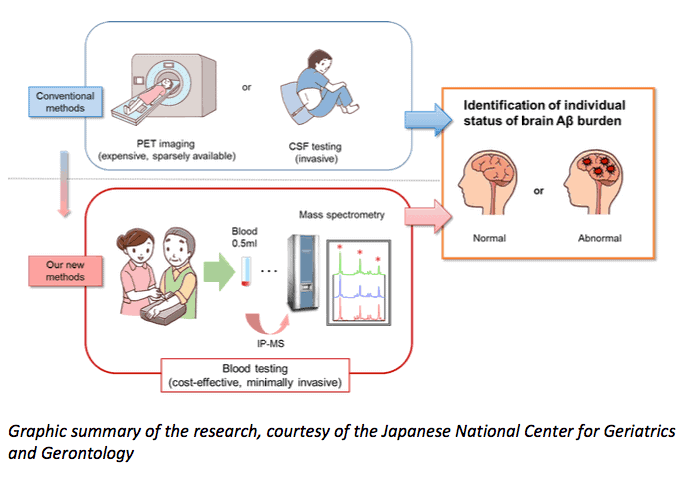
Current tests for beta-amyloid include brain scans with costly radioactive tracers, or analysing spinal fluid taken via a lumbar puncture. These are expensive and invasive, and generally only available in a research setting. A diagnosis is usually made without these tools, by assessing a patient’s range of symptoms.
Laureate Professor Colin Masters of the Florey Institute of Neuroscience and Mental Health, and The University of Melbourne, has been at the forefront of Alzheimer’s research since the 1980s. Professor Masters, who co-led the research published in the latest issue of Nature, says, “This new test has the potential to eventually disrupt the expensive and invasive scanning and spinal fluid technologies. In the first instance, however, it will be an invaluable tool in increasing the speed of screening potential patients for new drug trials.”
Background information and statistics (from Dementia Australia)
- 20-40% of the general elderly population over 70 years old have beta-amyloid buildup in their brain, and are considered to be “at risk” of developing Alzheimer’s disease at some future point.
- Dementia is the second leading cause of death of Australians contributing to 5.4% of all deaths in males and 10.6% of all deaths in females each year
- In 2016 dementia became the leading cause of death among Australian females, surpassing heart disease which has been the leading cause of death for both males and females since the early 20th century. Females account for 64.4% of all dementia related deaths
- Without a medical breakthrough, the number of people with dementia is expected to increase to 536,164 by 2025 and almost 1,100,890 by 2056
- In 2018, dementia is estimated to cost Australia more than $15 billion. By 2025, the total cost of dementia is predicted to increase to more than $18.7 billion in today’s dollars, and by 2056, to more than $36.8 billion
- The total estimated worldwide costs of dementia were US$818 billion in 2015
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!