Medications that mitigate inflammation caused by a variety of diseases including rheumatic arthritis may also compromise a person’s immune system, but a new approach points to a possible solution to this problem.
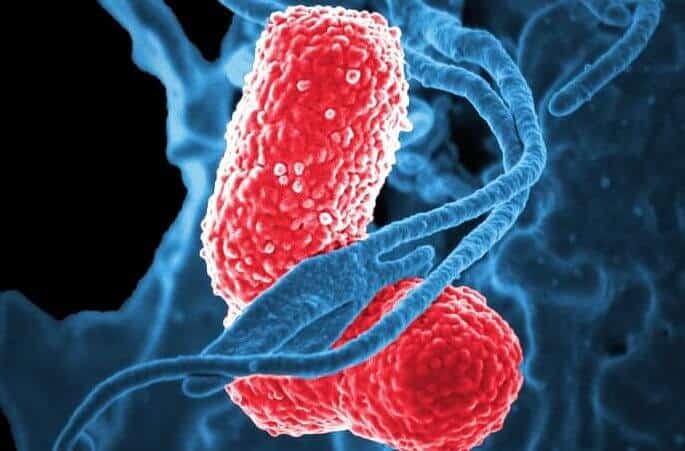
Researchers have discovered a mechanism that might alleviate inflammation by suppressing the migration of a type of white blood cells called neutrophils. The cells migrate within tissues in order to kill pathogens but may also cause excessive inflammation, resulting in tissue injury and other adverse effects.
The scientists identified a genetic molecule called miR-199, a type of “microRNA,” which reduces the migration of neutrophils, therefore potentially relieving inflammation without compromising the immune system.
“This is important because various challenges lie in the balance of dampening detrimental inflammation while preserving immunity,” said Qing Deng, an assistant professor in the Department of Biological Sciences at Purdue University.
The researchers used a genetic-screening method to identify eight microRNAs that suppress neutrophilic migration, including miR-199. They found that miR-199 directly suppresses the action of an enzyme called cyclin-dependent kinase 2, or CDK2, in turn dampening the migration of neutrophils.
Although CDK2 is well known for its role in regulating a cell’s life cycle – the process of a cell replicating its DNA and dividing to generate two cells — its link to neutrophil migration was previously unknown.
“This work suggests miR-199 and CDK2 as new targets for treating inflammatory ailments and introduces an avenue of the function for CDK2 outside the cell cycle regulation,” Deng said.
Findings are detailed in a paper appeared online this week in Proceedings of the National Academy of Sciences. Alan Y. Hsu, a doctoral student in Purdue’s Department of Biological Sciences, was the paper’s lead author. A complete listing of co-authors is available in the abstract.
Recently, microRNAs have been used in clinical trials to treat cancer and infection. They also are used as screening tools to identify the underlying mechanisms of diseases and cell behavior. However, the role of microRNAs in regulating neutrophil migration is largely unknown.
“The absence of this knowledge potentially leads to missed opportunities in harnessing microRNAs and their targets in restraining neutrophilic inflammation,” Deng said. “Our research results expand the current understanding of neutrophil migration and suggest a novel strategy to manage neutrophilic inflammation.”
The research was performed in zebrafish and also in human neutrophil-like cells.
“Our results reveal previously unknown functions of miR-199 and CDK2 in regulating neutrophil migration and provide a new direction in alleviating systemic inflammation,” Deng said.
The research has implications for diseases including rheumatic arthritis, diabetes, neurodegenerative diseases and cancer.
Findings showed miR-199 hinders neutrophil motility and directly targets CDK2. Although no previous studies have investigated the role of miR-199 in neutrophils, its role in suppressing inflammation and cell migration has been reported in cancer cells.
“Here, we provide evidence that miR-199 is a suppressor of cell migration in white blood cells, expanding its role beyond cancer biology,” Deng said.
Surprisingly, she said, miR-199 predominantly regulates the cell cycle-dependent kinase CDK2 in “terminally differentiated neutrophils.”
“When we say a cell is terminally differentiated that means the cell will not divide anymore,” she said. “The cell cycle is active in stem cells and cancer cells. But when cells change their gene expression to become neutrophils with immune-defense functions, they fight infections and die. So, it is unexpected that genes promoting cell cycle and cell division, such as CDK2, would regulate neutrophil function.”
The work is ongoing, and the next step is to understand the detailed molecular mechanisms for how CDK2 suppresses neutrophil migration and lethal inflammation.
The work aligns with Purdue’s Giant Leaps celebration, acknowledging the university’s global advancements made in health, longevity and quality of life as part of Purdue’s 150th anniversary. This is one of the four themes of the yearlong celebration’s Ideas Festival, designed to showcase Purdue as an intellectual center solving real-world issues.
The paper was co-authored by researchers affiliated with the Institute of Infection and Inflammation, Medical College of China Three Gorges University; Department of Medical and Molecular Genetics and Center for Computational Biology and Bioinformatics, Indiana University School of Medicine; Collaborative Core for Cancer Bioinformatics, Indiana University Simon Cancer Center; Department of Medical Microbiology and Immunology and Department of Pediatrics, University of Wisconsin–Madison; and Purdue’s Department of Agricultural and Biological Engineering, Weldon School of Biomedical Engineering, Institute for Inflammation, Immunology, and Infectious Disease, and Center for Cancer Research.
The research was funded by the National Institutes of Health (Grant R35GM119787 to Q.D., Grant R35GM118027 to A.H., Grant R01HD073156 to D.M.U., and Grant P30CA023168 to the Purdue Center for Cancer Research) for shared resources. Bioinformatics analysis was conducted by the Collaborative Core for Cancer Bioinformatics, shared by the Indiana University Simon Cancer Center (Grant P30CA082709) and the Purdue University Center for Cancer Research, with support from the Walther Cancer Foundation. Hsu is supported by the Purdue Research Foundation.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!