Researchers at the University of Maryland School of Medicine (UMSOM) found that targeting overactive immune cells in the brain with an experimental drug could limit brain cell loss and reverse cognitive and motor difficulties caused by traumatic brain injury (TBI). The findings, published Monday in the Journal of Neuroscience, suggest a potential new treatment for TBI and possibly other brain injuries.
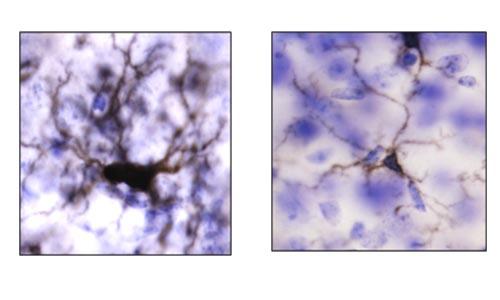
The UMSOM scientists administered a CSF-1R inhibitor for one week to mice beginning one month after TBI- a time at which animals have brain inflammation and neurological deficits. The researchers found the drug depleted more than 95 percent of the brain’s overactive immune cells (microglia) that are known to cause neurotoxic inflammation. Several weeks following the treatment, the cells had regenerated and the new cells were more similar to normal microglia, with less inflammatory features.
More importantly, the mice recovered markedly better than the control group that didn’t receive treatment, showing less loss of tissue and neurons with significantly better motor and cognitive performance.
“We were surprised to see that the extent to which such late treatment could reverse the inflammatory state and the cognitive effects of experimental TBI,” said study co-author Rebecca Henry, PhD, Research Associate in Anesthesiology at UMSOM. “This was a proof of concept study that depletion and subsequent repopulation of microglia cells after injury has a strong protective effect, but we clearly need more research to better understand this process before clinical translation.”
Both human and animal brains have specialized immune cells, called microglia, that protect against bacteria or viruses that enter the brain.
Evidence from previous clinical studies has shown an increase in microglia activation in patients who have suffered a moderate or severe traumatic brain injury. These changes appear to be correlated with neurological deficits in such patients, including cognitive function.
“These preclinical studies suggest that the consequences of TBI on brain degeneration and related neurological impairment may be modifiable quite long after injury,” said study co-author Alan Faden, MD, the David S. Brown Professor in Trauma at UMSOM. “We can potentially alter these effects by even highly delayed targeting of inflammatory pathways, a finding at odds with widely accepted views about treating head injury.”
The next step for the researchers is to isolate the microglia cells and use RNA resequencing techniques to learn more about which genes are driving inflammation and overactivation in order to better understand the mechanism identified in this study.
“This is an intriguing finding that points to an important role that inflammation plays in chronic debilitation from brain injuries,” said UMSOM Dean E. Albert Reece, MD, PhD, MBA, University Executive Vice President for Medical Affairs and the John Z. and Akiko K. Bowers Distinguished Professor. “Future studies will hopefully lead to new treatments for severe TBI that destroys a patient’s quality of life.”
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!