Patients with poorly controlled type 2 diabetes who underwent a novel, minimally invasive, endoscopic procedure called Revita® duodenal mucosal resurfacing (DMR) had significantly improved blood glucose (sugar) levels, liver insulin sensitivity, and other metabolic measures three months later, according to new data from the REVITA-2 study. These results, from a mixed meal tolerance test, have helped researchers verify the insulin sensitizing mechanism by which hydrothermal ablation of the duodenum improves blood sugar in patients with type 2 diabetes.
The research was accepted for presentation at ENDO 2020, the Endocrine Society’s annual meeting, and will be published in a special supplemental section of the Journal of the Endocrine Society.
“This outpatient procedure is being studied as the first disease-modifying therapy for type 2 diabetes and has thus far been demonstrated to be safe, effective, and durable through at least two years of follow up,” said study investigator, David Hopkins, MB.Ch.B. (M.D.), director of the Institute of Diabetes, Endocrinology and Obesity, King’s Health Partners in London, U.K.
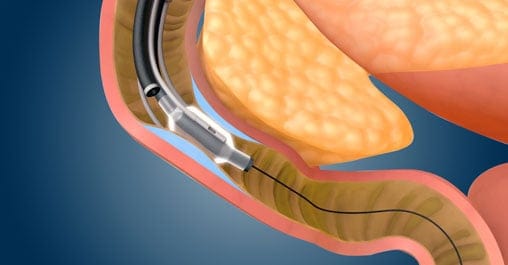
The REVITA-2 study, a randomized, sham-controlled clinical trial, explored the insulin-sensitizing mechanisms underlying the previously reported beneficial effects of the Revita DMR therapy, developed by Lexington, Mass.-based Fractyl Laboratories, sponsor of the study. The technology involves inserting a balloon catheter through the mouth and into the duodenum (upper small intestine) to precisely deliver thermal energy to the duodenal lining. Once treated, the damaged duodenal lining is flushed out, and a new mucosal layer begins to regenerate.
“The thickening of the duodenal mucosa (surface lining) occurs early in diabetes and may initiate changes in hormonal signaling that lead to insulin resistance, the main factor leading to type 2 diabetes,” Hopkins said. “By resurfacing the mucosa with the Revita DMR technique and effectively resetting this signaling, we are able to demonstrate a reduction of the insulin resistance underlying diabetes and associated metabolic complications.”
The researchers analyzed data from 70 patients (blinded: 35 treated; 35 sham) who had a meal tolerance test before and 12 weeks after a single endoscopic procedure. This test measures insulin secretion and insulin resistance by determining the insulin response to a “mixed meal,” which is a nutritional drink with a fixed amount of glucose and protein similar to a typical meal. The patients’ blood glucose levels were measured before the test (while fasting) and afterward.
The patients who received Revita DMR had a markedly improved glucose response, primarily driven by decreased fasting blood glucose levels, and had improved liver measures, suggesting better insulin action on the liver. Although the average fasting glucose level dropped by only 15 milligrams per deciliter (mg/dL) in the sham group, it fell by 41 mg/dL in the DMR-treated group. Hopkins said this suggests “a primary effect on insulin resistance.”
“These findings confirm that the duodenum is an important therapeutic target for type 2 diabetes,” Hopkins said. “The Revita treatment has the potential to transform the lives of patients who cannot adequately control their disease with drug therapies or who are interested in a non-drug treatment alternative that targets the root cause of metabolic disease.”
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!