A clinical trial has begun to evaluate whether the malaria drug hydroxychloroquine, given together with the antibiotic azithromycin, can prevent hospitalization and death from coronavirus disease 2019 (COVID-19). The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, is sponsoring the trial, which is being conducted by the NIAID-funded AIDS Clinical Trials Group (ACTG). Teva Pharmaceuticals is donating medications for the study.
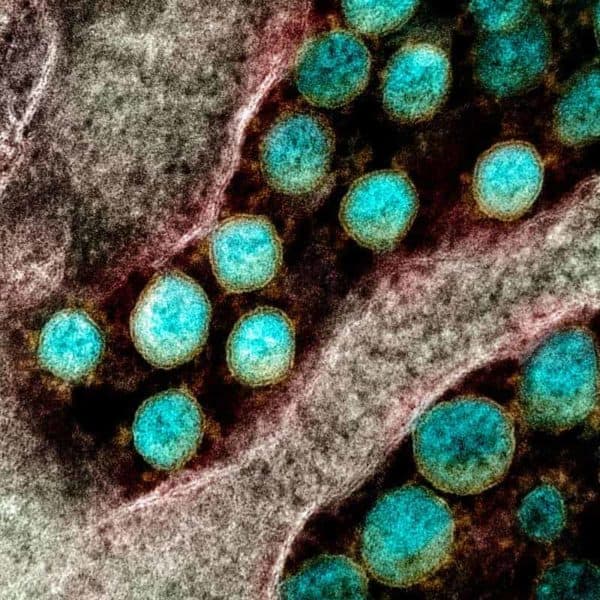
The Phase 2b trial will enroll approximately 2,000 adults at participating ACTG sites across the United States. Study participants must have confirmed infection with SARS-CoV-2, the virus that causes COVID-19, and be experiencing fever, cough and/or shortness of breath. The investigators anticipate that many of those enrolled will be 60 years of age or older or have a comorbidity associated with developing serious complications from COVID-19, such as cardiovascular disease or diabetes. Participants will be randomly assigned to receive short-term treatment with either hydroxychloroquine and azithromycin or matching placebos. People living with HIV and pregnant and breastfeeding women also are eligible to participate in the study. The first participant enrolled today in San Diego, California.
“We urgently need a safe and effective treatment for COVID-19. Repurposing existing drugs is an attractive option because these medications have undergone extensive testing, allowing them to move quickly into clinical trials and accelerating their potential approval for COVID-19 treatment,” said NIAID Director Anthony S. Fauci, M.D. “Although there is anecdotal evidence that hydroxychloroquine and azithromycin may benefit people with COVID-19, we need solid data from a large randomized, controlled clinical trial to determine whether this experimental treatment is safe and can improve clinical outcomes.”
As of May 13, the World Health Organization (WHO) has reported 4.17 million cases of and 287,399 deaths from COVID-19 worldwide. In the United States, 1.36 million confirmed COVID-19 cases and 82,246 deaths have been reported as of May 13, according to the Centers for Disease Control and Prevention (CDC).
Currently, there are no specific therapeutics approved by the U.S. Food and Drug Administration to treat people with COVID-19. Hydroxychloroquine is FDA-approved to prevent and treat malaria, as well as to treat the autoimmune diseases rheumatoid arthritis and lupus. Some preliminary reports have suggested that hydroxychloroquine, alone or in combination with the FDA-approved antibiotic azithromycin, may benefit people with COVID-19. Numerous clinical trials are planned or underway, including a recently launched study supported by NIH’s National Heart, Lung and Blood Institute evaluating the safety and effectiveness of hydroxychloroquine for treatment of adults hospitalized with COVID-19. On March 28, FDA issued an Emergency Use Authorization (EUA) to allow hydroxychloroquine and medical-grade chloroquine to be distributed from the Strategic National Stockpile and prescribed by doctors to hospitalized adolescents and adults with COVID-19, as appropriate, when a clinical trial is not available or feasible.
Participants in the ACTG study, called A5395, will receive oral medications to take at home. Those randomly assigned to the experimental treatment group will take 400 milligrams (mg) of hydroxychloroquine twice on the first day and 200 mg twice daily for an additional six days. They also will take 500 mg of azithromycin on the first day and 250 mg daily for an additional four days. The control group will receive equivalent numbers of placebo pills. Neither the participants nor the study team will know who received experimental treatment or placebo until the end of the trial.
Participants will record their symptoms, adherence to treatment, and major events such as hospitalizations in a diary for 20 days. Study staff will follow up with participants by telephone during this period. When possible, participants will come to the clinical research site for an in-person visit at day 20. Additional follow-ups will be conducted by telephone three and six months after treatment starts.
The main objective of the study is to determine whether hydroxychloroquine and azithromycin can prevent hospitalization and death due to COVID-19. Additionally, investigators will evaluate the safety and tolerability of the experimental treatment for people with SARS-CoV-2 infection. While hydroxychloroquine and azithromycin are both considered safe in most people, they can cause side effects ranging from headache and nausea to, rarely, heart rhythm problems that can be life-threatening. Because of the risk of heart problems when hydroxychloroquine is used alone or combined with azithromycin, FDA cautions that use of hydroxychloroquine for COVID-19 should be limited to clinical trials or for treating certain hospitalized patients under EUA so clinicians can monitor patients for adverse effects.
“This study will provide key data to aid responses to the COVID-19 pandemic,” said ACTG Chair Judith Currier, M.D., of the University of California, Los Angeles. “We are pleased to be able to leverage ACTG’s existing infrastructure for HIV treatment clinical trials to quickly implement this important study.”
The study team is led by Protocol Chair Davey Smith, M.D., of the University of California, San Diego. David Wohl, M.D., of the University of North Carolina at Chapel Hill, and Kara W. Chew, M.D., and Eric S. Daar, M.D., both of the University of California, Los Angeles, serve as protocol vice-chairs. The trial is expected to enroll quickly given the high incidence of COVID-19, and initial results may be available later this year.
For more information about A5395, visit ClinicalTrials.gov and search identifier NCT04358068. Adults interested in participating in the study should email [email protected].
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!