Gene therapy generally relies on viruses, such as adeno-associated virus (AAV), to deliver genes into a cell. In case of CRISPR-based gene therapies, molecular scissors can then snip out a defective gene, add in a missing sequence or enact a temporary change in its expression, but the body’s immune response to AAV can thwart the whole endeavor.
To overcome that obstacle, researchers at the University of Pittsburgh created a system that uses CRISPR in a different way. Their system briefly suppresses genes that are related to AAV antibody production so the virus can deliver its cargo unimpeded. These results published today in Nature Cell Biology.
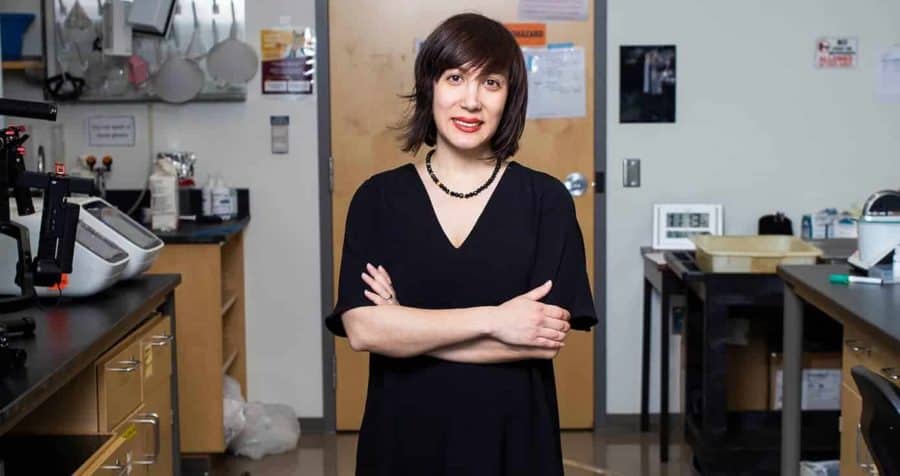
“Many clinical trials fail because of the immune response against AAV gene therapy,” said study co-senior author Samira Kiani, associate professor of pathology in Pitt’s School of Medicine and member of the Pittsburgh Liver Research Center (PLRC) and McGowan Institute for Regenerative Medicine. “And then you can’t readminister the shot because people have developed immunity.”
So Kiani and her long-time collaborator Mo Ebrahimkhani, associate professor of pathology at Pitt, member of PLRC and the McGowan Institute, set out to modify gene expression related to the body’s immune response to AAV. But this gene is important for normal immune function, so the researchers didn’t want to shut it down forever, just tamp it down momentarily.
Since CRISPR is such a convenient system for editing the genome, the pair figured they would put it to use for altering the master switches that orchestrate genes involved in immune response.
“We’re hitting two birds with one stone,” said Ebrahimkhani. “You can use CRISPR to do your gene therapy, and you can also use CRISPR to control the immune response.”
When the researchers treated mice with their CRISPR-controlled immune suppression system and then exposed them to AAV again, the animals didn’t make more antibodies against the virus. These animals were more receptive to subsequent AAV-delivered gene therapy compared to controls.
Beyond gene therapy, the study also shows that CRISPR-based immune suppression can prevent or treat sepsis in mice, highlighting the potential for this tool to be broadly useful for a range of inflammatory conditions, including cytokine storm and acute respiratory distress syndrome, both of which can crop up with COVID-19, though more studies are needed to engineer safety features.
“The main goal of this study was to develop CRISPR-based tools for inflammatory conditions,” said study lead author Farzaneh Moghadam, a PhD student in Kiani’s lab. “But when we looked at bone marrow samples, we saw that the group treated with our tool showed a lower immune response to AAV compared to the control group. That was very interesting, so we started exploring how this tool contributes to antibody formation against AAV and could potentially address safety and efficacy concerns with gene therapy trials.”
Kiani co-founded SafeGen Therapeutics with the goal of bringing this technology to the clinic.
This study was supported by National Institute of Biomedical Imaging and Bioengineering, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, and a DARPA Young Faculty Award.
Additional authors on the study include graduate student Ryan LeGraw and researcher Jeremy Velazquez from Pitt.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!