It saved lives in past epidemics of lung-damaging viruses. Now, the life-support option known as ECMO appears to be doing the same for many of the critically ill COVID-19 patients who receive it, according to an international study led by a University of Michigan researcher.
The 1,035 patients in the study faced a staggeringly high risk of death, as ventilators and other care failed to support their lungs. But after they were placed on ECMO—extracorporeal membrane oxygenation—their actual death rate was less than 40%. That’s similar to the rate for patients treated with ECMO in past outbreaks of lung-damaging viruses and other severe forms of viral pneumonia.
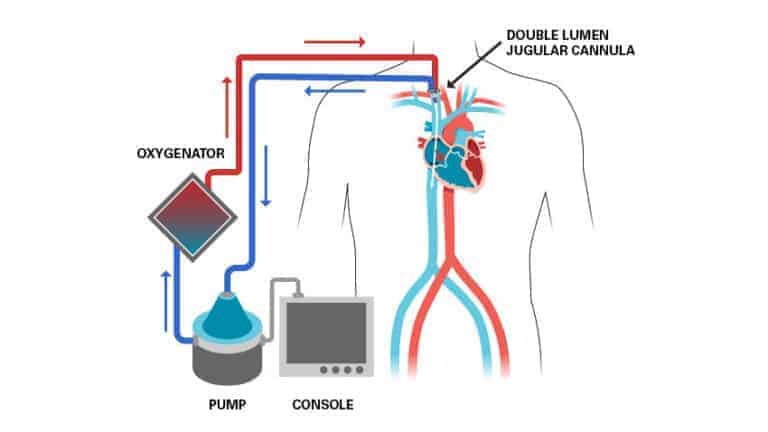
The new study published in The Lancet provides strong support for the use of ECMO in appropriate patients as the pandemic rages worldwide. It may help more hospitals that have ECMO capability understand which of their COVID-19 patients might benefit from the technique, which channels blood out of the body and into a circuit of equipment that adds oxygen directly to the blood before pumping it back into regular circulation.
Still, the international team of authors cautions that patients who show signs of needing advanced life support should receive it at hospitals with experienced ECMO teams, and that hospitals shouldn’t try to add ECMO capability mid-pandemic.
Global cooperation to achieve results
The study was made possible by a rapidly created international registry that has given critical care experts near real-time data on the use of ECMO in COVID-19 patients since early in the year.
Hosted by the Extracorporeal Life Support Organization (ELSO), the registry includes data submitted by the 213 hospitals on four continents whose patients were included in the new analysis. The study includes data on patients age 16 or older who were started on ECMO between January 16 and May 1, and follows them until death, discharge from the hospital, or August 5, whichever occurred first.
“These results from hospitals experienced in providing ECMO are similar to past reports of ECMO-supported patients, with other forms of acute respiratory distress syndrome or viral pneumonia,” says co-lead author Ryan Barbaro of Michigan Medicine, U-M’s academic medical center. “These results support recommendations to consider ECMO in COVID-19 if the ventilator is failing. We hope these findings help hospitals make decisions about this resource-intensive option.”
Co-lead author Graeme MacLaren of the National University Health System in Singapore said most centers in the study did not need to use ECMO for COVID-19 very often.
“By bringing data from over 200 international centers together into the same study, ELSO has deepened our knowledge about the use of ECMO for COVID-19 in a way that would be impossible for individual centers to learn on their own,” he said.
Insights into patient outcomes
Seventy percent of the patients in the study were transferred to the hospital where they received ECMO. Half of these were actually started on ECMO—likely by the receiving hospital’s team—before they were transferred. This reinforces the importance of communication between ECMO-capable hospitals and non-ECMO hospitals that might have COVID-19 patients who could benefit from ECMO.
The new study could also help identify which patients will benefit most if they are placed on ECMO.
“Our findings also show that mortality risk rises significantly with patient age, and that those who are immunocompromised, have acute kidney injuries, worse ventilator outcomes or COVID-19-related cardiac arrests are less likely to survive,” said Barbaro, who chairs ELSO’s COVID-19 registry committee and provides ECMO care as a pediatric intensive care physician at U-M’s C.S. Mott Children’s Hospital.
“Those who need ECMO to replace cardiac function as well as lung function also did worse. All of this knowledge can help centers and families understand what patients might face if they are placed on ECMO.”
Co-senior author Daniel Brodie of New York Presbyterian Hospital said the lack of reliable information early in the pandemic hampered the research team’s ability to understand the role of ECMO for COVID-19.
“The results of this large-scale international registry study, while hardly definitive evidence, provide a real-world understanding of the potential for ECMO to save lives in a highly selected population of COVID-19 patients,” said Brodie, who shares senior authorship with Roberto Lorusso of the Maastricht University Medical Center in the Netherlands and Alain Combes of Sorbonne University in Paris.
A robust statistical approach
Because the ELSO database does not track what happens to patients once they are discharged to home, other hospitals and long-term acute care or rehabilitation facilities, the study used a statistical approach based on in-hospital mortality up to 90 days after the patient was put on ECMO. This also allowed the team to account for the 67 patients who were still in the hospital as of August 5, whether they were still on ECMO, in the ICU or in step-down units.

The study tracked the outcomes for more than 1,000 patients for 90 days after they were placed on ECMO life support.
Philip Boonstra of the U-M School of Public Health, helped design the study using a “competing risk” approach, based on his experience handling the statistical design and analysis of long-term data from clinical trials for cancer.
“We used 90-day in-hospital mortality because this is the highest-risk period and because it allows us to use the information we have to the fullest, even if we don’t know the final outcome for every patient,” he said.
Having data through August, when only a small number of the patients in the study remained in the hospital, was important—though data are missing on a small number of patients. And even though patients who were discharged to their homes or a rehabilitation facility will likely have a long recovery ahead after the intensive level of care involved in ECMO, they are likely to survive based on past data. However, the fate of those who went to LTAC facilities, which provide long-term care at a near-ICU level, is less certain.
More about the study and next steps
More than half of the patients in the study were treated in hospitals in the United States and Canada, including Michigan Medicine’s own hospitals. U-M’s Robert Bartlett, emeritus professor of surgery and a co-author of the new paper, is considered a key figure in the development of ECMO, including the first use in adults in the 1980s. He led the development of the initial guidance for the use of ECMO in COVID-19.
“ECMO is the final step in the algorithm for managing life-threatening lung failure in advanced ICUs,” Bartlett said. “Now we know it is effective in COVID-19.”
As of Aug. 5, 380 of the patients in the study had died in the hospital, more than 80% of them within 24 hours of a proactive decision to discontinue ECMO care because of a poor prognosis. Of the remaining patients, 57% had gone home or to a rehabilitation center (311 patients) or had been discharged to another hospital or a long-term acute care center (277 patients). The rest were still in the hospital but had reached 90 days after the start of ECMO.
The new study adds to the information used to create the ECMO COVID-19 guidelines published by ELSO, which is in part based on past randomized controlled trials of ECMO’s use in ARDS.
Barbaro and others are studying the longer-term effects of ECMO care for any patient; he leads a team that has recently received a National Institutes of Health grant for a long-term study of children who have survived after treatment with ECMO.
Meanwhile, the ELSO registry continues to track the care of patients placed on ECMO because of COVID-19. Christine Stead, chief executive officer of ELSO, credits the rapid pivot and intense teamwork among ECMO centers and their staff for the strength of the new paper.
“We started with a WeChat dialogue with teams in China, who were able to share knowledge and help their counterparts in Japan be ready for the spread to their country,” she said. “We asked all the centers that take part in ELSO to change their practice, and begin entering data about patients as soon as they were placed on ECMO, rather than waiting until they were discharged from the hospital. This has allowed us to achieve something that will help hospitals make more informed decisions, based on meaningful data, as the pandemic continues.”
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!