Survival rates after a heart transplant are unaffected if the organ donor had used illicit drugs or died due to an overdose, a fact that is increasing the availability of hearts due to the rise in drug overdose deaths in the U.S., according to two new unrelated research studies published today in two of the American Heart Association’s scientific journals.
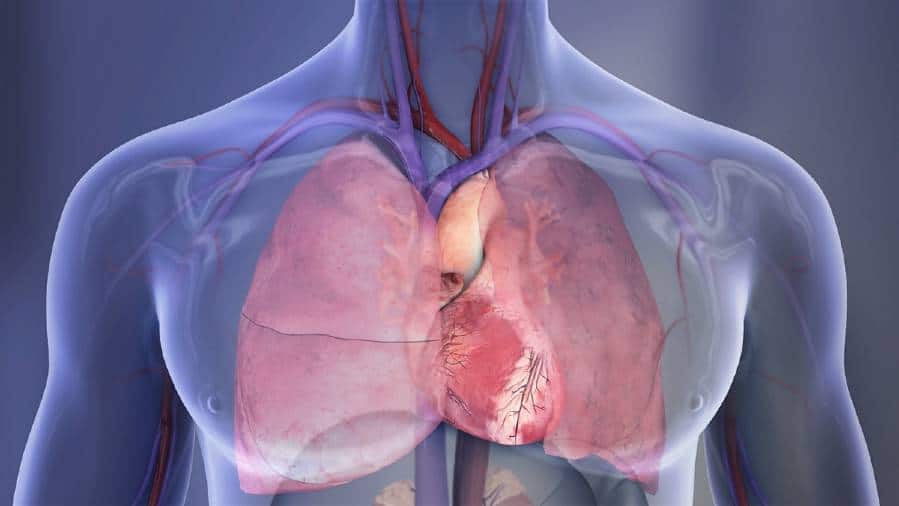
During a heart transplant, the patient’s failing heart is replaced with a healthy heart from a recently deceased donor. The most common reasons for a heart transplant are that one or both ventricles of the heart aren’t functioning properly or severe heart failure is present. In 2019, the United States recorded the highest number of heart transplants, with 3,552 transplantations performed. As of March 11, 2020, 3,661 people were on the waiting list for a heart transplant, and 52 people were on the waiting list for a heart and lung transplant, according to the American Heart Association’s 2021 Heart Disease and Stroke Statistical Update.
Data made available in 2019 found “no downside” to transplanting hearts from people who had used illicit drugs, and the practice has become routine, according to Howard Eisen, M.D., chair of the American Heart Association’s Heart Failure and Transplantation Committee of the Clinical Cardiology Council, who was not involved in either study.
“This research confirms previous data that these hearts – once considered high risk – are safe,” Eisen said. “These findings should encourage institutions who are not routinely using hearts from drug users to do so. It will reduce the waiting time and the number of deaths among people on the heart transplant waitlist.”
The first study, “Intoxicated Donors and Heart Transplant Outcomes: Long Term Safety,” reviewed data from 2007– 2017 and is published today in Circulation: Heart Failure, an American Heart Association journal.
Tragically, the opioid epidemic has led to an increase in potential heart donations, however, many of these hearts go unused due to the concern that the donor’s illicit drug use may decrease the chances of survival among heart-transplant recipients, explained lead study author David A. Baran, M.D., system director for advanced heart failure and transplantation at Sentara Heart Hospital in Norfolk, Virginia.
In the largest study to-date examining illicit drug use of heart transplant donors, and the only analysis to examine the toxicology data of donors obtained at hospital admission, Baran and colleagues reviewed nationwide information from the United Network for Organ Sharing (UNOS) database. They considered illicit drug use of donors in a comparison of survival after heart transplant for more than 23,000 adult, heart transplant recipients between January 1, 2007 to December 31, 2017. UNOS maintains a registry of all organ transplant activity in the United States and documents information about donors and recipients, including illicit drug use of the organ donors.
In this analysis, the average age of the heart donors was 32, and the average age of heart transplant recipients was 53. Using information from hospital urine tests before the donors died, the researchers identified the type and number of illicit drugs the donors had used, including opioids, cocaine, methamphetamine, alcohol, marijuana, barbiturates, amphetamines, phencyclidine (PCP) and others. Researchers noted that alcohol use appeared to decline over the decade of the analysis period, while all other drug use increased.
Baran and colleagues found that the percentage of transplant recipients who survived was comparable between transplant recipients who received a heart from a donor who used any illicit drugs and those whose donors did not use drugs. For example, the percentage of surviving heart transplant patients whose donors used opioids and those whose donors did not was about 90% after one year; about 77% at five years and roughly 60% at 10 years. The findings were comparable for other types of illicit drugs, even among heart donors who tested positive for multiple—five or more—illicit drugs.
“We thought that illicit drugs like cocaine or methamphetamine, which can lead to heart attacks, would prove to be dangerous,” Baran said. “However, we were wrong. We should not reject a heart from a donor just because they used one or more illicit drugs.”
The main limitation is that the study included only those hearts that were accepted for transplantation. Other limitations include the medical administration of opioids in the hospital could be misleading, the possibility of errors when information was entered into the database and the lack of a central laboratory to confirm the results submitted by local laboratories.
Co-authors are Justin Lansinger, B.A.; Ashleigh Long, M.D., Ph.D.; John M. Herre, M.D.; Amin Yehya, M.D.; Edward J. Sawey, M.D.; Amit P. Badiye, M.D.; Wayne Old, M.D.; Jack Copeland, M.D.; Kelly Stelling, R.N.; and Hannah Copeland, M.D. The study received no external funding.
The second study, “National Trends in Heart Donor Utilization Rates: Are We Efficiently Transplanting More Hearts?” compared data from 2003-2007 to 2013-2017. The article published today in the Journal of the American Heart Association, an open access journal of the American Heart Association.
Researchers from Wisconsin suggest that broader acceptance of hearts from donors who died due to a drug overdose or donors who had hepatitis C could alleviate the strain on the current waitlist for a heart transplant.
“We hope that patients who are awaiting transplants are encouraged to accept hearts from donors who had hepatitis C or who died due to a drug overdose, if their health care team finds the donor heart to be an appropriate match,” said lead study author Ravi Dhingra, M.D., M.P.H., medical director of the heart failure and transplant program and associate professor of medicine at the University of Wisconsin-Madison.
Dhingra and colleagues explored if the donor pool should include people who have died due to a drug overdose or who had hepatitis C. Hepatitis C is a viral liver infection that spreads through contact with contaminated blood, such as from shared needles; from mother to infant during pregnancy and delivery; or due to an organ transplant from someone infected with hepatitis C. Because the infection can be treated with the advent of new, direct-acting, antiviral medications, hepatitis C is much more manageable, leading to an increase in availability of organs from donors who had hepatitis C.
They noted that physicians are required to obtain separate consents from patients regarding acceptance of hepatitis C-donor organs and prior authorization from health insurance carriers to cover the cost of hepatitis C medications, if needed by the transplant recipient.
“About 20% of patients on the heart-transplant waiting list die while waiting to receive a transplant or become too sick to remain good transplant candidates,” Dhingra said.
Dhingra and colleagues accessed the UNOS database to compare the number of donor hearts accepted or declined for transplant from 1995 through 2018. They compared heart transplant recipients’ survival from donors who died from a drug overdose or had hepatitis C to survival from donors who had not died of a drug overdose or had hepatitis C.
Compared to organ heart donors from 2003-2007, donors in 2013-2017 were older, weighed more, were more likely to have high blood pressure and diabetes and to have used illicit drugs, which increases the risk for hepatitis C. However, compared to 2003-2007, the risk of death among transplant recipients in 2013-2017 was 15% lower one month after the heart transplant and 21 percent lower one year later.
The study reviewed major additional risk factors among transplant recipients that could have affected survival after the heart transplant, although it could not prove cause and effect between donor or recipient characteristics and post-transplant survival.
Co-authors are Naga Dharmavaram, M.D.; Timothy Hess, Ph.D.; Heather Jaeger, R.N.; Jason Smith, M.D.; Joshua Hermsen, M.D.; and David Murray, M.D. The study was funded by the Health Resources and Services Administration and the National Heart, Lung, and Blood Institute of the National Institutes of Health.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!