A research collaboration including scientists from Oregon State University has developed a new technology to help surgeons know where a patient’s nerves are, lessening the chance of nerve damage.
The technology is based on hydrogels, three-dimensional networks of polymers that absorb and retain large amounts of water, and takes aim at a surgical complication that’s widespread and persistent. Depending on the procedure, OSU’s Adam Alani says, a patient can face a double-digit percentage chance of sustaining a nerve injury.
For example, he notes, people needing their thyroid gland removed are looking at a 15% likelihood of voice changes resulting from damage to their recurrent laryngeal nerves. Apply those odds to the 12% of the United States’ population that is likely to develop a thyroid condition, for which thyroidectomy is a common treatment, and the numbers for that type of operation alone are staggering.
“Nerve sparing techniques have been around for decades, but nerve identification and sparing remain a big challenge, with success rates strongly correlated with an individual surgeon’s skill and experience,” said Alani, a researcher in the OSU College of Pharmacy. “Intraoperative nerve damage affects all surgical specialties and represents a significant problem even for surgeries that are performed all of the time like prostatectomies, hysterectomies, hernia repair and thyroidectomies.”
Alani, an adjunct faculty member at Oregon Health & Science University, worked with OHSU colleague Summer Gibbs on the study, funded by the National Institutes of Health. Findings were published in Biomaterials.
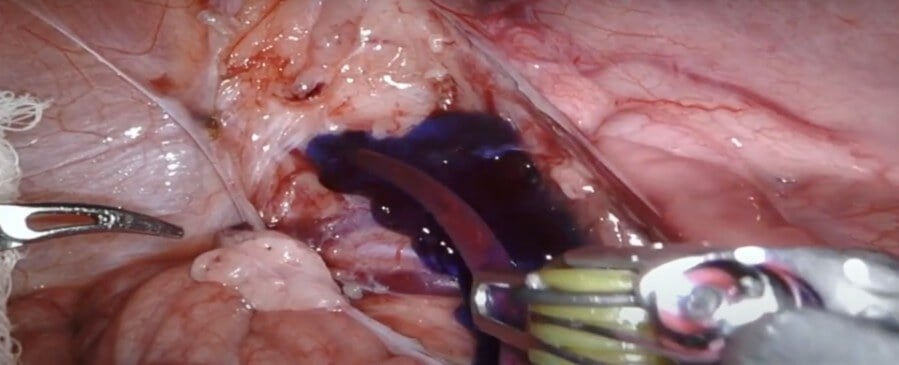
The research is an important step toward improving a nerve sparing technique called fluorescence guided surgery, or FGS. Specific tissues, in this case nerves, can be better detected if they fluoresce – i.e., emit light after absorbing light or some other kind of electromagnetic radiation.
For the tissues to do that, they need to be treated with a fluorophore, microscopic molecules that absorb and send out light of specific wavelengths.
Collaborating with scientists at OHSU and Intuitive Surgical, Alani’s lab developed an effective hydrogel fluorophore based on compounds called pluronics. Also known as poloxamers, pluronics are polymers synthesized by the condensation of ethylene oxide and propylene oxide.
“Hydrogels have been successfully used to deliver contrast agents in imaging technologies like MRI and CT scans,” Alani said. “And pluronics are already used as a drug delivery agent in products approved by the Food and Drug Administration. The physical characteristics of our pluronics-based formulation allow for nerve-specific stain solution to be applied with relative ease as a liquid, and then it stays in place after it almost instantly forms a gel.”
Successful testing in two animal models – mouse and pig – suggests the new technology is “a clinically viable method for fluorescence guided nerve sparing during thyroidectomy as well as other procedures,” Alani said.
And because pluronics already have FDA approval, the technology is eligible for fast-tracked regulation under the agency’s guidelines for “exploratory investigational new drugs.” The guidelines allow for early phase 1 clinical trial exploratory approaches involving safe microdoses of potential drug candidates, enabling researchers to move ahead more quickly than usual.
“Directly administering a contrast agent in the treatment area is an attractive alternative to systemic administration of fluorescent probes,” Alani said. “Selectively labeling tissues only within the surgical field requires a significantly lower dose than systemic administration.”
Vidhi Shaw, Adel Al-Fatease and Syed Zaki Husain Rizvi of the OSU College of Pharmacy also contributed to the study.
Alexander Antaris and Jonathan Sorger represented Intuitive Surgical, developer of the widely used robotic da Vinci Surgical System with which the new technology is compatible, Alani said.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!