A study conducted by NYU Grossman School of Medicine reveals a correlation between episodes of systemic lupus erythematosus, an autoimmune disease, and increased growth of a specific gut bacterium, Ruminococcus blautia gnavus. The research tracked the disease flare-ups and bacterial blooms in 16 women with lupus of diverse racial backgrounds over a four-year period. The study identified 34 genes associated with the bacterium’s growth in individuals with inflammation. Antibodies in lupus patients showed a strong affinity for specific bacterial lipoglycan molecules, known triggers of inflammation. The findings highlight the role of R. gnavus in lupus and may guide the development of new treatments to prevent or treat flares.
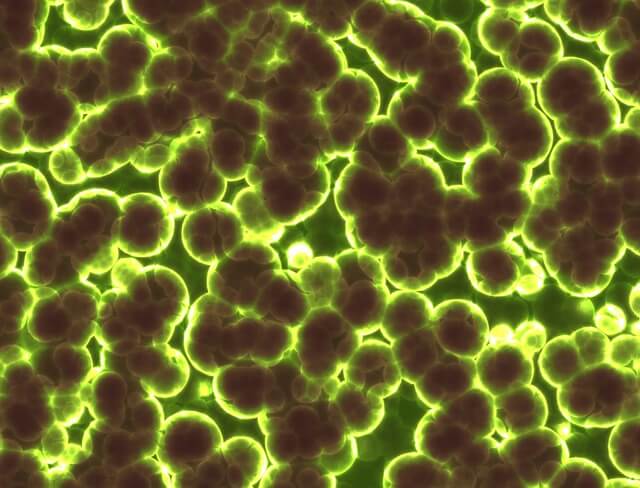
A recent study conducted by NYU Grossman School of Medicine reveals a significant association between episodes of systemic lupus erythematosus (lupus) and increased growth of a specific gut bacterium called Ruminococcus blautia gnavus. The study, conducted over a four-year period, tracked disease flare-ups and bacterial blooms in 16 women with lupus of diverse racial backgrounds.
The research findings indicate that bacterial blooms of R. gnavus occurred simultaneously with disease flare-ups in five out of the 16 lupus patients. Systemic lupus erythematosus involves damaging inflammation, particularly in the kidneys, as well as joints, skin, and blood vessels. Four of the patients with R. gnavus blooms had severe cases of lupus nephritis, the most common form of the disease that specifically affects the kidneys, while one patient had a severe form involving inflammation in multiple joints.
The study, published in the Annals of Rheumatic Diseases, identified 34 genes associated with the growth of R. gnavus in individuals with inflammation. Although the precise causes of lupus, which affects around 1.5 million Americans, remain unknown, many experts suspect that bacterial imbalances trigger inherited genetic factors responsible for the disease.
The researchers also examined how tightly the patients’ immune system antibodies bound to structures in the bacterial wall, similar to their response to an invading virus. These antibodies showed a strong affinity for specific bacterial lipoglycan molecules known to trigger inflammation. These lipoglycans were found to be common in R. gnavus strains in lupus patients but not in healthy individuals. Antibodies play a major role in the body damage caused by lupus, and this diagnostic antibody response highlights the important role played by R. gnavus in the autoimmune disease.
Lead investigator of the study, Doua Azzouz, PhD, states, “Our findings provide the strongest evidence to date that silent growths of Ruminococcus blautia gnavus are tied to active serious renal disease in lupus patients.”
The study also revealed a common bacterial link among a racially diverse group of females with various forms of lupus. Lupus is more prevalent in women than in men and affects more individuals from Black, Hispanic, and Asian backgrounds compared to White individuals.
Study senior investigator and immunologist Gregg Silverman, MD, explains, “Our goal is to use our growing understanding of the biological pathways that underpin the disease to develop new treatments that prevent or treat flares for all forms of lupus.”
The researchers suggest that future treatments for lupus, especially lupus nephritis, could potentially focus on decreasing the use of immune system-dampening drugs and instead promote the use of less-toxic antibacterial agents, probiotics, or dietary regimens that prevent imbalances in the gut bacterial population or microbiome, such as Ruminococcal blooms.
Previous research by Silverman’s team demonstrated that R. gnavus blooms weaken the gut wall barrier, leading to bacterial leakage, which triggers inflammatory and overactive immune responses.
Silverman and the research team plan to expand their research to include more patients from other medical centers. They also intend to conduct further experiments in mouse models of lupus to understand how R. gnavus colonization triggers lupus and whether the blooms affect the severity and frequency of flares and inflammation.
The researchers aim to conduct experiments on various lipoglycan molecules from different R. gnavus strains to determine if specific parts of the molecular structure play a key role in triggering inflammation. They also plan to investigate if other lipoglycans prompt an immune response associated with lupus or other gut-related diseases, such as Crohn’s disease.
For the study, researchers collected stool and blood samples from lupus patients being treated at NYU Langone. The participants were closely monitored for disease flare-ups. Test results were compared with those of 22 female volunteers of similar age and racial background who did not have lupus and were in good health.
Systemic lupus erythematosus, as an autoimmune disease, can cause widespread inflammation and long-term tissue damage in affected organs. Approximately half of lupus patients develop lupus nephritis, and a quarter of them may experience end-stage renal disease, requiring regular blood dialysis and potentially kidney transplantation.
The study received funding support from National Institute of Health grants, the Lupus Research Alliance, the Judith and Stewart Colton Autoimmunity Center at NYU Langone, and the P. Robert Majumder Charitable Trust.
Apart from Silverman, other NYU Langone researchers involved in the study include Ze Chen, Peter Izmirly, Lea Ann Chen, Zhi Li, Chongda Zhang, Adriana Heguy, Davis Mieles, Kate Trujillo, Alejandro Pironti, Gregory Putzel, David Fenyo, and Jill Buyon. Study co-investigators are Dominik Schwudke and Nicolas Gisch from the Leibniz Lung Center in Borstel, Germany, and Alexander Alekseyenko from the Medical University of South Carolina in Charleston.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!