Scientists at Washington University in St. Louis have developed an innovative real-time monitor capable of detecting SARS-CoV-2 virus variants in an indoor environment within approximately 5 minutes.
Combining recent advancements in aerosol sampling technology and an ultrasensitive biosensing technique, the device offers a cost-effective solution for detecting COVID-19 in real-time and has the potential to monitor other respiratory virus aerosols such as influenza and respiratory syncytial virus (RSV). The breakthrough research, published in Nature Communications on July 10, showcases the remarkable sensitivity and versatility of the monitor.
The interdisciplinary team of researchers, hailing from the McKelvey School of Engineering and the School of Medicine, comprises Rajan Chakrabarty, Joseph Puthussery, John Cirrito, and Carla Yuede. Chakrabarty, the Harold D. Jolley Career Development Associate Professor of energy, environmental & chemical engineering, played a pivotal role in leading the project.
The monitor addresses the critical need for assessing the safety of indoor spaces in real-time, as highlighted by Cirrito: “There is nothing at the moment that tells us how safe a room is. If you are in a room with 100 people, you don’t want to find out five days later whether you could be sick or not. The idea with this device is that you can know essentially in real-time, or every 5 minutes, if there is a live virus.”
The research team built upon a micro-immunoelectrode (MIE) biosensor previously developed by Cirrito and Yuede, which detected amyloid beta as a biomarker for Alzheimer’s disease. They explored the feasibility of converting the biosensor into a detector for SARS-CoV-2, a process that involved replacing the antibody recognizing amyloid beta with a nanobody derived from llamas. This nanobody effectively recognizes the spike protein found in the SARS-CoV-2 virus. The small size, ease of reproduction and modification, and low cost of the nanobody contributed to its selection.
“The nanobody-based electrochemical approach is faster at detecting the virus because it doesn’t need a reagent or a lot of processing steps,” explains Yuede. “SARS-CoV-2 binds to the nanobodies on the surface, and we can induce oxidation of tyrosines on the surface of the virus using a technique called square wave voltammetry to get a measurement of the amount of virus in the sample.”
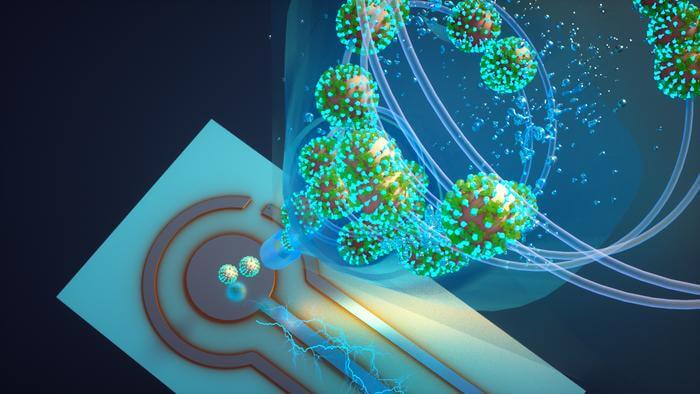
To integrate the biosensor effectively, Chakrabarty and Puthussery incorporated it into an air sampler utilizing wet cyclone technology. This sampler operates by introducing high-velocity airflow mixed with fluid, creating a surface vortex that traps virus aerosols. The fluid collected by the automated pump is then directed to the biosensor for seamless virus detection via electrochemistry.
Chakrabarty highlights the superiority of their wet cyclone sampler, stating, “The high virus recovery by the wet cyclone can be attributed to its extremely high flow rate, which allows it to sample a larger volume of air over a 5-minute sample collection compared with commercially available samplers.” The team’s monitor boasts a flow rate of approximately 1,000 liters per minute, making it one of the highest flow-rate devices on the market. Compact and easily deployable, the monitor measures about 1 foot wide and 10 inches tall. When a virus is detected, it illuminates, alerting administrators to enhance airflow or circulation in the room.
To validate their invention, the researchers tested the monitor in the apartments of two COVID-positive patients. The air samples collected from the patients’ bedrooms were compared with those from a virus-free control room, utilizing real-time PCR. The results confirmed the detection of RNA from the virus in the air samples from the infected bedrooms, while the control samples exhibited no traces of the virus.
In further laboratory experiments, where SARS-CoV-2 was aerosolized in a chamber mimicking a room, the wet cyclone and biosensor successfully detected varying levels of airborne virus concentrations within minutes of sampling.
While the primary focus has been SARS-CoV-2, the team envisions extending the monitor’s capabilities to measure other pathogens such as influenza, RSV, and rhinovirus. In a hospital setting, the monitor could even be used to detect staph or strep, known to cause complications for patients. As Cirrito emphasizes, this breakthrough technology could have a significant impact on public health.
The team is now working towards commercializing this revolutionary air quality monitor, ensuring widespread access to real-time virus detection in indoor environments.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!