Allergic transfusion reactions (ATRs), a potentially life-threatening side effect of blood transfusions with unclear mechanisms, may be linked to food allergies in pediatric patients as per a recent study by scientists from Japan.
They found that ATRs may be triggered by the presence of allergens in the donor’s blood, influenced by their pre-donation diet. These findings could pave the way for safer blood transfusions through the development of preventive measures and countermeasures for ATRs.
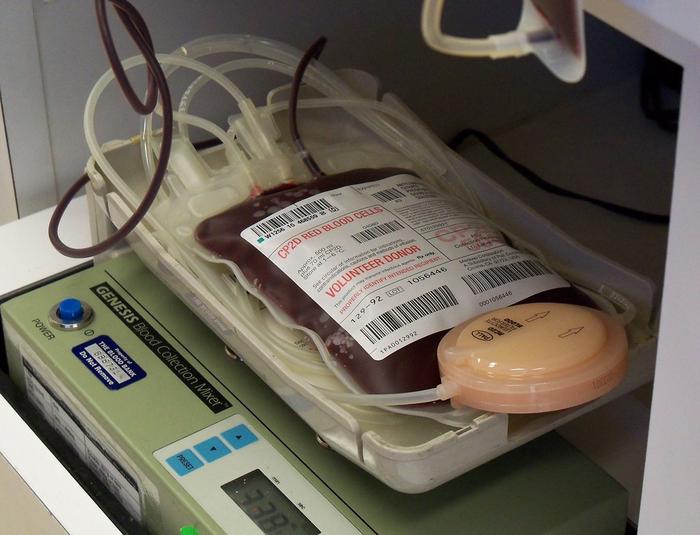
Blood transfusions are often life-saving procedures in various medical settings. They are required not only after severe blood loss due to surgery or trauma but also as standard treatment for certain blood disorders like anemia and sickle cell disease. However, blood transfusions can have serious side effects, with allergic transfusion reactions (ATRs) being particularly prevalent among children. Although scientists believe ATRs are caused by immunoglobulin E (IgE)-mediated type 1 allergy (or “immediate hypersensitivity”), the responsible allergens are not always known.
Against this backdrop, a research team composed of Dr. Ryu Yanagisawa of Shinshu University Hospital, Japan, alongside Dr. Minoru Tozuka and Dr. Yasunori Ito from Nagano Children’s Hospital, Japan, set out to find more answers. In their latest study, published online in the journal Allergy on January 11, 2024, the researchers focused their attention on what might have appeared to be an unlikely suspect. Dr. Yanagisawa, who led the study at the University’s Division of Blood Transfusion, explains: “In our previous study, we found that pediatric patients with food allergies were characteristically more prone to ATRs. Considering that food allergies are also more prevalent in children, we decided to investigate whether the food the donor ate before giving blood could be associated with the development of ATRs in children with food allergies.”
Between May 2022 and December 2023, the researchers collected blood samples from over 100 pediatric patients with diagnosed food allergies toward either eggs, wheat, or milk. They also collected blood from two healthy donors before and after substantial ingestion of these food products and extracted the serum. Shortly after collecting blood from each allergic patient, the researchers conducted basophil activation tests (BATs) by exposing the sample to the corresponding sera. As the name implies, these tests assess the activation of basophils, a particular type of white blood cell that is strongly involved in allergic reactions.
Interestingly, in patients with egg allergy, BAT levels were significantly higher when the blood was exposed to the serum of donors who had ingested eggs. Moreover, serum obtained from blood donor samples collected four hours after egg ingestion resulted in markedly higher BAT levels than those collected two hours after egg ingestion. In contrast, the results for milk and wheat were more varied, with BAT levels only being elevated after exposure to the serum of one of the two donors.
To gain deeper insights and lend more weight to the results, the researchers decided to run BAT tests with sera from sixteen additional donors. “Although some differences were observed among donors, blood samples obtained after egg ingestion generally activated basophils in cases of egg allergy with high egg white-specific IgE levels,” comments Dr. Yanagisawa. “Similarly, elevated BAT levels in patients with milk and wheat allergies were also associated with allergen-specific IgE levels.”
Overall, the evidence obtained through this study strongly suggests that ATRs could be triggered by the food consumed by donors prior to a blood donation. Although further analyses and experiments will be needed to confirm this with more certainty, these efforts constitute a necessary first step towards elucidating the mechanisms underlying ATRs. “In future, it could be possible to predict in advance who is likely to suffer from an ATR. Given enough time, preventive measures and countermeasures to ATRs could be developed, leading to safer blood transfusions,” concludes Dr. Yanagisawa.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!