Study shows behavior not affected by perceptions of risk
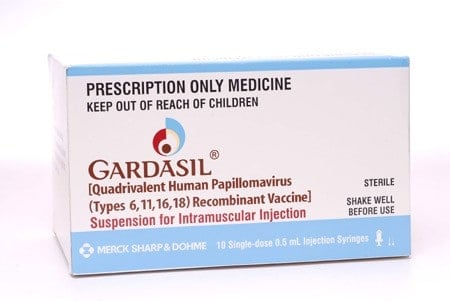
A new study may alleviate concerns that the human papillomavirus (HPV) vaccine leads to either the initiation of sex or unsafe sexual behaviors among teenage girls and young women.
The Cincinnati Children’s Hospital Medical Center study shows that teen girls’ and young women’s beliefs regarding the HPV vaccine, whether accurate or inaccurate, are not linked to subsequent sexual behaviors over the six months after vaccination. Those enrolled in the study didn’t change their behavior whether they thought safer sex was less important or just as important after vaccination, or whether they thought the vaccine did or did not decrease the risk of sexually transmitted infections (STIs) other than HPV. The vast majority thought it was still important to practice safer sex after vaccination, and most did not believe that HPV vaccination protected against other STIs.
The study is published in the eFirst pages of the journal Pediatrics.
“We hope this study reassures parents, and thus improves HPV vaccination rates, which in turn will reduce rates of cervical and other cancers that can result from HPV infection,” says Jessica Kahn, MD, a physician in the division of adolescent medicine at Cincinnati Children’s.
Dr. Kahn studied sexually experienced and inexperienced young teens and women between the ages of 13 and 21. More than 300 completed questionnaires immediately after receiving the vaccine, and most of them completed follow-up surveys again two and six months later. These surveys assessed demographics, knowledge and attitudes about the HPV vaccine, beliefs about risk for acquiring an STI other than HPV after vaccination, beliefs about the need for safer sexual behaviors after vaccination, and sexual behaviors. These behaviors included sexual initiation among those who were sexually inexperienced at the time of vaccination, number of sexual partners, and having sexual intercourse without a condom among those who were sexually experienced at the time of vaccination.
HPV is a common STI that affects 7.5 million girls and young women in the United States between the ages of 14 and 24. HPV causes cervical cancer and other genital cancers, but vaccines are available that prevent the types of HPV that are responsible for 70 percent of cervical cancers. The U.S. Advisory Committee on Immunization Practices recommends HPV vaccination for teenage girls and women between the ages of 11 and 26, for teen boys and men between 11 and 21, and for men 22 to 26 who are at high risk for HPV.
Perhaps because of concerns that vaccination of adolescents could lead to risky sexual behaviors, vaccination coverage among 13- to 17-year-old girls increased from 48.7 percent in 2010 to only 53.8 percent in 2012 for one dose of the vaccine. Coverage increases from 32 percent to only 33.4 percent for three doses over the same time period.
“Data demonstrating that HPV vaccination does not lead to riskier behaviors will allow clinicians to provide accurate, evidence-based information to address the concerns of parents and thereby increase vaccination rates,” says Dr. Kahn.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!