The first direct proof of a long-suspected cause of multiple HIV-related health complications was recently obtained by a team led by the University of Pittsburgh Center for Vaccine Research (CVR). The finding supports complementary therapies to antiretroviral drugs to significantly slow HIV progression.
The study, which will be published in the June issue of the Journal of Clinical Investigation and is available online, found that a drug commonly given to patients receiving kidney dialysis significantly diminishes the levels of bacteria that escape from the gut and reduces health complications in non-human primates infected with the simian form of HIV. The study was funded by the National Institutes of Health (NIH).
“We now have direct evidence of a major culprit in poor outcomes for some HIV-infected people, which is an important breakthrough in the fight against AIDS,” said Ivona Pandrea, M.D., Ph.D., professor of pathology at Pitt’s CVR. “Researchers and doctors can now better test potential therapies to slow or stop a key cause of death and heart disease in people with HIV.”
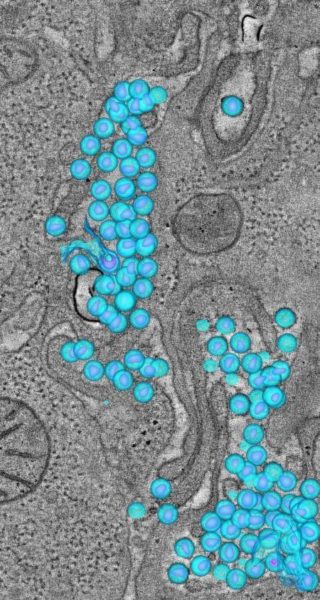
Chronic activation of the immune system and inflammation are major determinants of progression of HIV infection to AIDS, and also play an important role in inducing excessive blood clotting and heart disease in HIV patients. Doctors believed this was due to microbial translocation, which occurs when bacteria in the gut gets out into the body through intestinal lining damaged by HIV. However, no direct proof of this mechanism existed.
Dr. Pandrea and her colleagues showed blocking the bacteria from leaving the intestine reduces the chronic immune activation and inflammation. They did this by giving the drug Sevelamer, also known by the brand names Renvela and Renagel, to monkeys newly infected with simian immunodeficiency virus, or SIV, the primate-form of HIV.
Sevelamer is an oral drug approved by the U.S. Food and Drug Administration to treat elevated levels of phosphate in the blood of patients with chronic kidney disease.
The gut bacteria bind to Sevelamer, making it much more difficult for the bacteria to escape into the body and cause serious problems, such as heart disease, while further weakening the immune system and allowing HIV to progress to full-blown AIDS.
In SIV-infected monkeys treated with Sevelamer, levels of a protein that indicates microbial translocation remained low. However, in the untreated monkeys the levels increased nearly four-fold a week after SIV infection.
The treated monkeys with the lower rates of microbial translocation also had lower levels of a biomarker associated with excessive blood clotting, showing that heart attacks and stroke in HIV patients are more likely associated with chronic immune system activation and inflammation, rather than HIV drugs.
“These findings clearly demonstrate that stopping bacteria from leaving the gut reduces the rates of many HIV comorbidities,” said Dr. Pandrea.
Because most interventions in people infected with HIV begin after the person has reached chronic stages of infection when the gut is already severely damaged, Dr. Pandrea notes, “These treatments may not be as effective later in the infection. Clinical trials in HIV-infected patients were not yet successful in reducing microbial translocation in chronically infected patients. Our study points to the importance of early and sustained drug treatment in people infected with HIV.”
Other approaches, such as coupling Sevelamer with antibiotics, anti-inflammatory drugs, probiotics or supplementation of existing HIV/AIDS drugs could further reduce the likelihood of microbial translocation. Clinical trials are underway to assess these strategies.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!