The use of electronic alerts by hospitals treating patients with acute kidney injury may increase interventions without improving care, a study by Yale researchers found.
The study was published Feb. 25 in The Lancet.
Acute kidney injury (AKI) is a serious condition that can lead to dialysis and even death in hospitalized patients. To prevent these adverse outcomes, some hospital systems have proposed using electronic alerts to detect the condition at an early stage. To test the effectiveness of an alert system, first author Dr. F. Perry Wilson, assistant professor of medicine at Yale, and his co-authors conducted a randomized trial with 2,400 patients at the Hospital at the University of Pennsylvania in Philadelphia.
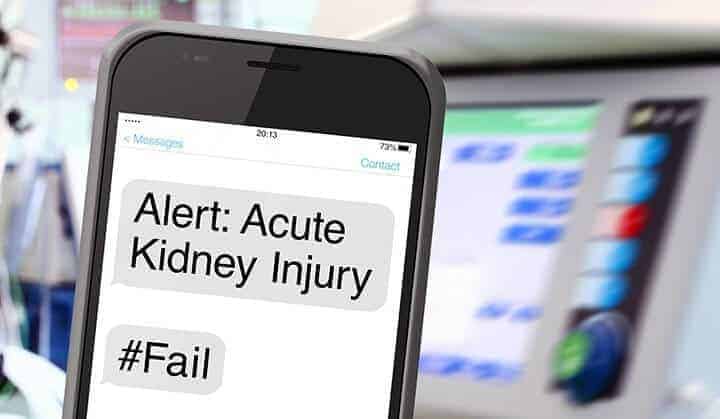
The researchers randomized patients into one of two study groups: an AKI alert group and a “usual care” group with no alert. When a patient tested positive for AKI — determined by serum creatinine values — the provider and a pharmacist received an alert in the form of a text page informing them of the diagnosis and encouraging them to take appropriate steps. The message also included a link to a website with guidelines for managing AKI.
The researchers reviewed outcomes of the alert system at 7, 14, and 30 days after hospital admission. At the end of the eight-month study period, they were surprised by their findings.
“Our hypothesis was that it would improve outcomes,” said Wilson. “But we found that, overall, there was no effect. Informing the doctors did not change behavior, and it did not change outcomes in terms of dialysis or death.”
One reason may be because AKI is a condition with no clear-cut treatments, Wilson suggested. “I think we put this tool into the clinicians hands and didn’t teach them how to use it.”
While the alert system did not improve outcomes, in a subset of patients it did increase interventions, including more renal consultations and dialysis. These interventions, however, did not correlate with higher-quality care. “For acute kidney injury, more treatment is not necessarily better,” Wilson noted.
The study findings are notable because hospital systems, including the National Health Service in the United Kingdom, are moving toward increased use of electronic alerts. “We concluded that for AKI the alerts are ineffective,” Wilson said.
Other Yale authors Dr. Jeffrey Testani, Dr. Chirag R Parikh; additional authors are Dr. Michael Shashaty, Dr. Iram Aqeel, Yuliya Borovskiy, Susan Ellenberg, Dr. Harold I. Feldman, Dr. Hilda Fernandez, Dr. Yevgeniy Gitelman, Dr. Jennie Lin, Dr. Dan Negoianu, Dr. Peter P. Reese , Richard Urbani, and Dr. Barry Fuchs.
This work was funded in part by K23DK097201 and a Penn Center for Healthcare Improvement and Patient Safety Pilot Grant to FPW, K23HL114868 and L30HL115790 to JT, T32DK007006 to JL.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!