-An international study led by researchers from Université Laval and CHU de Québec-Université Laval has identified significant vascular changes in the brains of people with Huntington’s disease. This breakthrough, the details of which are published in the most recent issue of Annals of Neurology, will have significant implications for our understanding of the disease and could open the door to new therapeutic targets for treating this fatal neurodegenerative condition.
Huntington’s disease (HD) is a hereditary neurodegenerative disorder that causes serious motor, cognitive, and psychiatric dysfunction and gradually leads to loss of autonomy and death. The disease develops in people age 40 to 50 on average. There is no cure and current treatments can only help control certain symptoms, but do not slow the neurodegenerative process. The disease affects roughly 1 in 10,000 people.
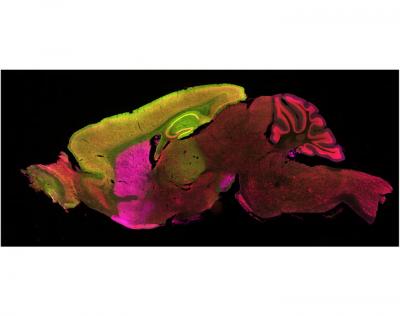
Although scientists have long known the cause of Huntington’s disease, little is known about the physiological processes associated with it. Certain neurological diseases, such as Parkinson’s and Alzheimer’s, are accompanied by changes in the vasculature of the brain and in the blood-brain-barrier, the interface that controls exchanges between the blood and the central nervous system. The team led by Francesca Cicchetti, professor at the Université Laval Faculty of Medicine and researcher at CHU de Québec-Université Laval, examined the brains of people affected by HD or who had died from it as well as a murine model of the disease to determine whether these changes are also present in Huntington’s disease.
The data collected shows the presence of mutant huntingtin, the protein responsible for the disease, in all major components of the brain’s blood vessels. Affected brains also show higher blood vessel density and reduced blood vessel diameter. “The abnormalities observed within the cerebral blood vessels were accompanied by an increased permeability of the blood-brain-barrier, which could allow the pathological protein to propagate from the peripheral to the central nervous system,” Professor Cicchetti noted.
“At the moment, we are still uncertain as to how this contributes to the development or progression of the disease,” Professor Cicchetti added. “However, these results, along with our observations published in the same journal last year, strongly suggest that the disease is not solely the result of a phenomenon that is intrinsic to the cells–i.e., the product of a genetic mutation–but rather that healthy cells can also be infected by the mutant protein.”
These findings open up new avenues for treating Huntington’s disease. “If indeed the transport of the mutant protein is facilitated by an increased permeability of the blood-brain-barrier, we could consider developing therapies aimed at reestablishing its integrity and preventing diseased peripheral cells from migrating to the brain,” the researcher concluded.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!