The survival and proliferation of usually harmless Escherichia coli in the gut of inflammatory bowel disease patients may now be better understood, as researchers have defined a fundamental mechanism through which the bacteria can thrive during flare-ups.
Some strains of E. coli normally live in the intestines of humans, and are important for a healthy digestive tract. However, for people who suffer from inflammatory bowel diseases (IBD), these innocuous strains may proliferate during a flare-up and further contribute to disease and discomfort.
According to the Centers for Disease Control, over 1 million Americans suffer from IBD, which includes a broad range of gastrointestinal tract problems such as Crohn’s disease and ulcerative colitis.
“Several types of inflammatory bowel disease are characterized by expansion of the opportunistic E. coli in the gut,” said Matam Vijay-Kumar, assistant professor of nutritional sciences and medicine at Penn State. “However, the mechanisms by which E. coli can thwart the hostile host innate immune system are poorly understood. Identifying these mechanisms will help to reduce the E. coli burden in the inflamed gut and prevent chronic extra-intestinal diseases.”
Vijay-Kumar and colleagues studied the interactions between enterobactin, myeloperoxidase and lipocalin 2 and how they regulate E. coli in the intestine and report their findings today (May 12) in Nature Communications.
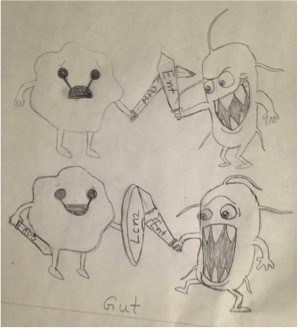
Enterobactin (Ent) is an iron-loving chemical secreted by E. coli that takes iron from host proteins in the body and aids the proliferation of E. coli. Myeloperoxidase (MPO) is an antibacterial protein that white blood cells produce to fight bacteria. However, Ent inhibits MPO from doing its job.
Lipocalin 2 (Lcn2) is another protein, also produced by white blood cells, that gathers up Ent — so that bacteria fail to obtain a sufficient amount of iron for their survival. The researchers found that Lcn2 can counter the effects of Ent on MPO.
“These bacteria can be harmful under special circumstances, such as IBD,” said Vijay-Kumar. “Most E. coli express enterobactin, a siderophore, and to avoid its recognition by the host lipocalin 2, they have the flexibility to express stealth siderophores. Strictly speaking, chelation of iron in the gut by enterobactin and inhibition of host MPO at the same time is positive for E. coli and negative for the host.”
With this study, the researchers say, they have defined a new defense mechanism used by E. coli residing in a human or animal host — the inhibition of MPO by Ent.
“We have to find a way to identify the drugs which can inhibit or degrade secreted enterobactin,” said Vijay-Kumar. “Alternatively, since MPO is known to be pro-inflammatory not only in IBD but also in other inflammatory diseases, it may be possible to develop enterobactin-based drugs to alleviate inflammatory pathways.” The National Institutes of Health supported this research.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!