Following a heart attack or other heart trauma, the heart is unable to replace its dead cells. Patients are often left with little option other than heart transplants, which are rarely available, or more recently cell therapies that transplant heart cells into the patient’s heart. In far too many cases, however, the transplanted heart cells do not engraft well, resulting in poor recovery.
One reason for the engraftment problem is the quality of the heart cells. For a typical cell therapy, heart cells are made from different stem cells, but the quality of the heart cells will vary. In particular, the maturation of the heart cells will be different. “Cells of different maturation will be mixed and transplanted together,” said Dr. Shunsuke Funakoshi, a scientist at the Center for iPS Research and Applications (CiRA), Kyoto University, and first author of a new study that investigated the optimal maturation of heart cells for the transplant, leading him to wonder if maturation is a factor in engraftment.
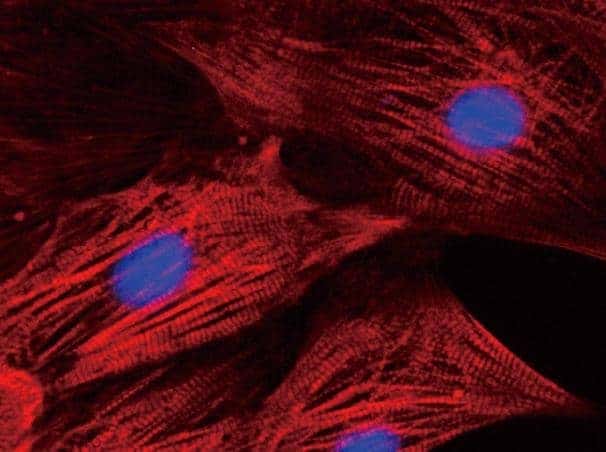
Under the direction of Senior Lecturer Yoshinori Yoshida, Funakoshi took induced pluripotent stem (iPS) cells that were reprogrammed from skin cells and made them into heart cells. Heart cells differentiated from iPS cells effectively go through all stages of development. “Heart cells at different stages could behave very differently,” said Fukakoshi. He therefore prepared heart cells of different maturation and transplanted them into damaged hearts of living mice. Hearts that received cells differentiated for 20 days showed much better engraftment than those that received cells differentiated for more or less, suggesting there exists an optimal maturation stage for cell therapies. However, Funakoshi cautions which day for human patients cannot be determined from this study. “We need to test animals bigger than mice,” he said.
Currently, over a billion cells are needed for human heart cell therapies. Knowing which cells are best for the therapy should not only improve patient outcome, but also reduce the number of cells required, which would further reduce both the time of the preparation and invasiveness of the procedure.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!