A groundbreaking imaging study at USC has identified specific brain networks responsible for urinary control that malfunction in stroke survivors, offering new hope for treating a common yet often overlooked complication.
The research, published this month in the journal Stroke, reveals that a network of brain regions known as the “salience network” fails to activate properly in stroke survivors experiencing urinary incontinence – a condition affecting up to 79% of patients immediately after stroke and persisting in nearly 40% one year later.
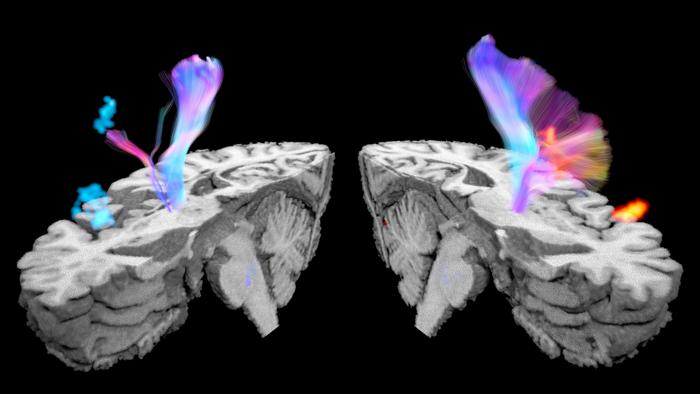
Using an innovative functional magnetic resonance imaging (fMRI) technique, researchers observed brain activity during both voluntary and involuntary bladder emptying, making this the first study to identify distinct neural patterns during incontinent episodes.
“The brain plays a crucial role in regulating the bladder, allowing people to sense bladder fullness and giving them the ability to delay urination until it is socially appropriate or initiate it at will,” explained Dr. Evgeniy Kreydin, lead author and adjunct assistant professor of clinical urology at the Keck School of Medicine of USC.
“In contrast, stroke survivors often struggle to suppress unwanted bladder contractions and may even lose bladder sensation and awareness entirely,” Kreydin noted.
The condition goes beyond mere inconvenience. Medical records show that post-stroke incontinence predicts poorer recovery outcomes, including higher mortality rates and increased disability – yet it remains undertreated in many clinical settings.
What makes this study particularly valuable is its methodological innovation. Rather than the traditional approach of having participants enter an MRI scanner with a full bladder, researchers developed a system to observe repeated filling and emptying cycles while simultaneously recording both brain activity and bladder pressure.
“In contrast to previous studies where participants using a catheter entered the scanner with a full bladder and voided on command, our study enabled us to observe filling and voiding repeatedly,” said Kay Jann, PhD, imaging expert from the USC Mark and Mary Stevens Neuroimaging and Informatics Institute. “The simultaneous recording of bladder pressure allowed us to identify both voluntary and involuntary bladder emptying. This allowed us to detect differences in brain activity during involuntary emptying for the first time.”
The findings revealed a stark contrast. During voluntary urination, both healthy individuals and stroke survivors showed significant activation in brain regions associated with sensorimotor control and decision-making. However, during involuntary bladder emptying in stroke survivors, researchers observed minimal brain activation, suggesting a breakdown in the neural networks controlling urination.
Most notably, the study identified the salience network – a collection of brain regions that evaluate the importance of internal bodily signals – as a crucial component in preventing incontinence. While this network activated properly during bladder filling in healthy individuals and during voluntary urination in stroke survivors, it remained inactive when stroke survivors experienced involuntary urination.
This neural signature could become the target for new treatment approaches, including non-invasive brain stimulation techniques, medications enhancing neural activation, or cognitive training designed to improve voluntary control.
The findings earned Dr. Kreydin the prestigious McGuire-Zimskind Award from the Society of Urodynamics, Female Pelvic Medicine, and Urogenital Reconstruction for his significant contributions to the field.
Dr. Charles Liu, director of the USC Neurorestoration Center and senior author of the study, believes this research opens doors for developing targeted therapies. “The neurological basis of urination is still poorly understood, and additional research will be crucial for the neurorestoration of the urinary and reproductive systems,” said Liu. “This work not only deepens our understanding of a common post-stroke complication but also provides hope for a better quality of life for millions of stroke survivors globally.”
The multidisciplinary research team included urologists, neurosurgeons, and imaging experts from Keck School of Medicine of USC, Keck Medicine of USC, the Rancho Los Amigos National Rehabilitation Center, and the Shirley Ryan Ability Lab.
While currently focused on understanding the mechanisms of post-stroke incontinence, researchers hope future studies will explore how different types of strokes affect urinary control and whether early interventions targeting the salience network might prevent chronic incontinence – ultimately restoring dignity and improving quality of life for the millions affected by this challenging condition.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!