For four decades, HIV has remained virology’s grandmaster, outmaneuvering every attempt to develop a protective vaccine. The virus’s bewildering mutation rate—which lets it alter its appearance faster than our immune system can recognize it—combined with its ability to hide its most vulnerable parts, has thwarted even the most sophisticated scientific approaches. Now, a carefully orchestrated pair of clinical trials suggests researchers may have found a way to speak directly to the rare immune cells capable of seeing through HIV’s disguises.
The studies, published May 15 in Science, represent a conceptual turning point in vaccine development: rather than simply presenting the immune system with viral fragments and hoping for the best, scientists have engineered a precision approach that guides specific immune cells through a developmental journey toward producing broadly neutralizing antibodies—the specialized defenders that can recognize HIV despite its chameleon-like mutations.
Vaccines That Whisper to Rare Immune Cells
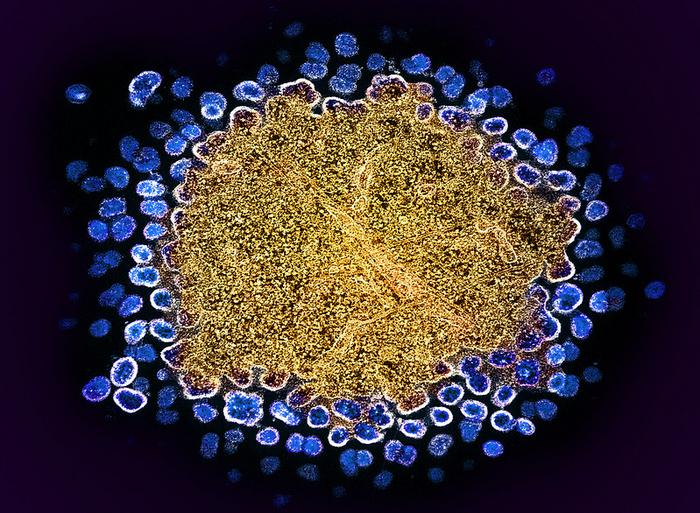
Inside your body right now are billions of B cells, each programmed to produce a unique antibody. Only an infinitesimal fraction—perhaps one in 300,000—have the genetic potential to develop into producers of the broadly neutralizing antibodies needed to combat HIV. The researchers’ audacious goal: find these needles in the haystack, activate them, and then coach them through a maturation process.
Two clinical trials—IAVI G002 with 60 participants in North America and IAVI G003 with 18 participants in Rwanda and South Africa—tested whether an mRNA-based vaccine strategy could find and nurture these rare immune cells. The results offer the first clinical evidence that this stepwise development of specialized immune responses is possible in humans.
“We’ve now shown in humans that we can initiate the desired immune response with one shot and then drive the response further forward with a different second shot. We’ve also shown that the first shot can work well in African populations,” says William Schief, professor at Scripps Research and executive director of vaccine design at IAVI’s Neutralizing Antibody Center, who led the international research effort.
What separates this approach from conventional vaccines is its exquisite specificity—like a teacher who knows precisely which student needs which lesson. Called “germline targeting,” it first activates only those B cells with the right genetic features, then guides them through progressive mutations that bring them closer to producing the desired broadly neutralizing antibodies.
A Delicate Choreography of Prime and Boost
The researchers found that when participants received a priming vaccine followed by a distinctly different booster shot—a technique known as heterologous boosting—their immune systems were effectively guided through the early stages of antibody development. The priming shot activated the rare target cells, while the booster pushed them further along their developmental path.
This sequential strategy yielded surprising results:
- All 17 North American participants receiving this prime-then-boost regimen developed VRC01-class antibodies—early precursors to the broadly neutralizing antibodies needed against HIV
- Over 80% developed what researchers termed “elite” responses, characterized by multiple beneficial mutations that move these antibodies closer to broadly neutralizing capability
- Counterintuitively, giving just one primer before the booster proved more effective than two primers—suggesting more isn’t always better in immune education
Meanwhile, in the African trial, which tested only the priming vaccine, 94% of participants showed successful activation of these rare immune cells, demonstrating the approach’s potential in populations with the greatest HIV burden.
“These incredibly exciting results underscore the importance and capability of global partnerships to drive cutting-edge science,” says Julien Nyombayire, executive director of the Center for Family Health Research in Kigali, Rwanda, and one of the lead investigators of the African trial.
The Language Barrier Between Vaccines and Our Immune System
To appreciate why this matters requires understanding the fundamental problem of HIV vaccine development. Our immune system’s antibodies recognize specific shapes, like a lock recognizing a key. But HIV rapidly changes these shapes, making yesterday’s antibody useless against today’s virus.
Some extremely rare antibodies, however, recognize parts of HIV that cannot change without compromising the virus’s ability to function—like spotting a criminal by identifying features they cannot disguise. These broadly neutralizing antibodies typically develop only after years of infection, too late to prevent initial infection.
Mark Feinberg, President and CEO of IAVI, underscores the significance: “These remarkable results validate the rational vaccine design that underpins this approach. A vaccine would be a tremendous step forward for global health and could help bring an end to the HIV pandemic.”
The Unexpected Price of Precision
Despite the promising immune responses, the trials revealed an unexpected challenge: 18% of North American participants experienced skin reactions like itching and hives, with 10% developing symptoms lasting more than six weeks. These reactions, while generally mild or moderate and ultimately treatable, were notably more common than those seen with other mRNA vaccines.
Curiously, the African trial showed a different safety profile, with no cases of hives reported—raising intriguing questions about potential biological or environmental differences that might influence vaccine responses across populations.
The Winding Road Ahead
How much closer does this bring us to an actual protective HIV vaccine? The answer lies in understanding what these trials were not designed to do. They didn’t attempt to produce the final broadly neutralizing antibodies needed for protection, nor did they test whether participants were protected against HIV infection.
Instead, they demonstrated something arguably more fundamental: that the human immune system can be methodically guided through the early stages of a complex developmental process that might eventually lead to broadly neutralizing antibodies. It’s like teaching someone the alphabet and basic vocabulary of a language—not yet fluency, but the critical foundation.
A follow-up study is already planned in South Africa to evaluate lower vaccine doses, which might maintain effectiveness while reducing side effects. Beyond HIV, this precision approach to vaccine development could potentially revolutionize how we address other stubborn pathogens that have resisted conventional vaccines.
After decades of disappointments in HIV vaccine research, these trials suggest we may finally be learning how to speak the complex language of immune development—a dialogue that could ultimately lead to protection against one of humanity’s most persistent viral adversaries.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!