New research shows that even when skin symptoms improve with modern biological treatments, many psoriasis patients still have persistent inflammation throughout their bodies. This lingering inflammation appears strongly connected to obesity and fatty liver disease, potentially explaining why psoriasis patients face higher risks of cardiovascular problems despite successful skin treatment.
The findings, published in the Journal of Investigative Dermatology, could reshape how doctors approach psoriasis treatment by highlighting the need to address the whole-body aspects of the disease rather than focusing solely on clearing skin symptoms. The international study examined over 200 patients across three countries who had achieved good skin clearance with biologic medications.
What happens when inflammation persists beneath the surface, invisible to both patient and physician, yet continues affecting vital organs? This question formed the core of the researchers’ investigation.
The Hidden Inflammation Problem
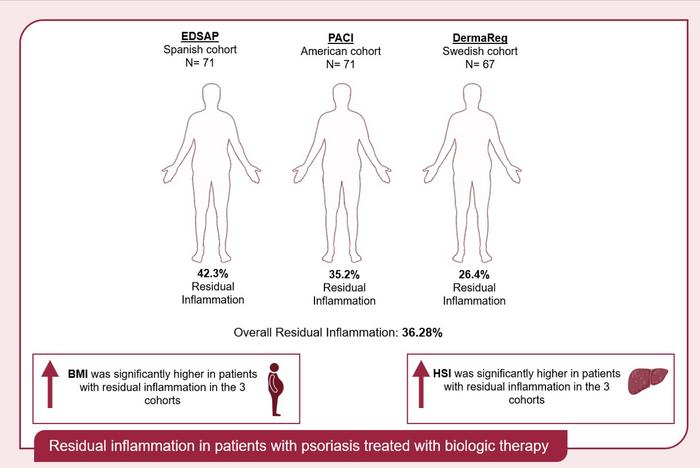
The prospective observational study followed 209 psoriasis patients from Spain, the United States, and Sweden who had achieved excellent skin clearance (minimal or no visible psoriasis) while on biologic therapy. Despite their skin improvement, researchers found that 36.3% of these patients still had what they term “residual inflammation,” as measured by elevated C-reactive protein (CRP), a key marker of inflammation in the blood.
“Patients with psoriasis have a reduced life expectancy due to an increased risk of cardiovascular disease. With the goal of better understanding this, we wanted to explore psoriasis as a systemic disease and its broader health implications,” explains lead investigator Álvaro González-Cantero, MD, PhD, from the Department of Dermatology at Hospital Universitario Ramón y Cajal in Madrid.
This persistent inflammation could help explain why psoriasis patients face higher cardiovascular risks even when their skin symptoms are well-controlled. The research is the first to comprehensively assess this concept across multiple international populations.
Key Findings from the Study
- 36.3% of patients maintained elevated inflammation markers despite excellent skin clearance
- Patients with residual inflammation had significantly higher BMI (body mass index) and waist circumference
- Fatty liver disease markers were consistently elevated in patients with lingering inflammation
- Women were more likely than men to have persistent inflammation across all three study groups
- Certain biologic medications (anti-TNF drugs) appeared more effective at reducing systemic inflammation
- Body imaging showed increased inflammation in the liver, bone marrow, and spleen of affected patients
Obesity and Fatty Liver Disease Connection
The researchers found that patients with residual inflammation had consistently higher BMI and waist measurements across all three study cohorts. Additionally, these patients showed increased markers for metabolic dysfunction-associated steatotic liver disease (MASLD), previously known as non-alcoholic fatty liver disease.
Using advanced imaging techniques in the American cohort, the researchers observed that patients with residual inflammation had significantly higher inflammation levels in the liver, bone marrow, and spleen. They also had greater volumes of both visceral (around organs) and subcutaneous (under skin) fat tissue.
“Our present study offers novel insights into psoriasis management by characterizing residual inflammation in patients undergoing biologic therapy across three independent international cohorts,” Dr. González-Cantero noted. “This is particularly important now because it highlights that despite achieving good skin responses with biologics, a significant subset of patients, predominantly those with obesity (especially central obesity), higher baseline systemic and organ inflammation, increased subcutaneous and visceral adipose tissue, and markers of MASLD, continue to exhibit residual inflammation.”
Implications for Patient Care
The findings suggest that doctors treating psoriasis should look beyond skin improvement when assessing treatment success. Patients with risk factors like obesity or fatty liver disease may need additional monitoring and interventions to address their full-body inflammation.
Co-first author Alba Lecumberri, MD, from Hospital Universitario Ramón y Cajal in Madrid, explained the practical implications:
“The strong association identified between residual inflammation and obesity, particularly central obesity and markers of hepatic inflammation, suggests that these patients may benefit from a more intensive cardiovascular risk assessment and management. This could involve closer monitoring of inflammatory markers like high-sensitivity C-reactive protein, as well as parameters related to liver health, by integrating lifestyle modifications or weight management strategies.”
Commenting on the study, Michael Garshick, MD, MBBS, from New York University Grossman School of Medicine, added: “This research emphasizes the elevated cardiovascular risk in patients with psoriasis and that dermatologists (and rheumatologists) should be at the forefront of recognizing the cardiometabolic and cardiovascular concerns in the psoriasis patient population. An elevated high-sensitivity C-reactive protein testing can be used to further refine assessment of which psoriasis may be candidates for both lipid lowering and weight loss treatments.”
Looking Forward
The researchers believe this study represents an important step toward understanding psoriasis as more than just a skin disease. By defining the concept of “residual inflammation” in psoriasis, they hope to spark a broader approach to treatment that addresses both visible and invisible aspects of the condition.
Emilio Berna-Rico, MD, PhD, co-first author from Hospital Universitario Ramón y Cajal, concluded: “We believe this to be a relevant study for dermatology, as it has assigned the term ‘residual inflammation’ for the first time in psoriasis patients, taking into account the systemic inflammation of the disease. We hope that our results can pave the way for a broader approach in psoriasis research, which will allow us to mitigate the effects of systemic inflammation and improve patient management through the use of the innovative therapies available to us, in addition to educating patients on a healthy and anti-inflammatory lifestyle, in collaboration with other healthcare professionals.”
Joel M. Gelfand, MD, MSCE, from the University of Pennsylvania Perelman School of Medicine and Deputy Editor for the Journal of Investigative Dermatology, summed up the significance: “Despite excellent control of skin disease, a substantial percentage of psoriasis patients demonstrate residual systemic inflammation. These findings emphasize that just treating the skin signs of psoriatic disease is not sufficient, and patients often need additional approaches to lowering systemic inflammation.”
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!