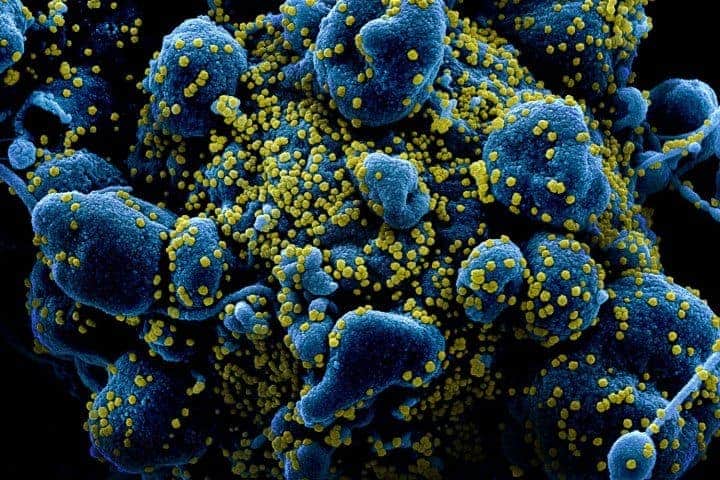
Patients with severe COVID-19 produce antibodies that paradoxically shut down their immune system’s virus-fighting response just when they need it most, according to new UC San Francisco research published in Nature.
Scientists believe this overzealous antibody response is an inappropriate engagement of an ancient biological feedback circuit whose real function is to help the body tamp down levels of immune signaling molecules called interferons, to modulate the immune response once a viral infection is under control.
Interferons help to stop a cell’s protein-making machinery, so viruses can’t hijack it to make copies of themselves. But in patients with severe COVID-19, antibodies that block the effects of interferons appear prematurely, removing the cells’ defenses while the infection is still raging.
The antibodies lock onto a cell surface protein called CD32b, which functions as a primal “off” switch for interferons. By closely examining immune cell populations in 21 patients, researchers found that severe patients – whom they defined as those needing mechanical ventilation or intensive care in the hospital – were unable to produce a line of interferon-stimulated immune cells that were abundant in the patients who had mild or moderate disease.
To further demonstrate that it was really the antibody blockade of the surface receptor that was preventing the formation of these protective interferon-stimulated cells, the researchers bathed healthy immune cells in serum containing antibodies from the severe patients. The healthy immune cells promptly lost their ability to respond to interferon, either partially or completely.
But when the scientists removed the antibodies from the serum, the healthy immune cells were once again able to normally differentiate into the interferon-stimulated immune cells. Likewise, when they blocked the CD32b receptor to prevent the antibodies from turning off the interferon signaling circuit, the cells were able to respond to interferons.
This is not the first study to implicate interferons in severe COVID-19 disease. Previous research demonstrated that 12 percent of severe patients have an autoimmune reaction against their own interferons, which also neutralizes it. The UCSF research shows how the remaining 88 percent of severe COVID-19 patients may be experiencing a different, more global immune breakdown that also involves antibodies made by their immune system in its attempt to control the virus.
Scientists said the discovery of this mechanism of severe disease opens up new approaches to developing therapies that could prevent it.
“What we’re learning here is how to address the mistakes of the immune system with immunotherapy,” said Matthew “Max” Krummel, PhD, an immunologist and professor in the UCSF Department of Pathology who led the effort with colleagues at UCSF’s Bakar ImmunoX Initiative, CoLabs and the COMET Consortium. “It’s another way to handle the immune system. Rather than pre-educating it with a vaccine, you prevent the immune system from going off the rails after a person gets infected.”

Krummel, whose work usually focuses on the immune system off-switches that are targeted by the cancer immunotherapy agents called checkpoint inhibitors, said a similar approach also could be taken to combat the worst effects of both COVID and other viral infections.
“An immunotherapy for a pandemic would be a breakthrough in how we drug a pathogen,” he said. “You don’t just target the pathogen, but instead change how the immune system responds to it – just like we did for cancer.”
The faulty mechanism could be targeted with existing antibody treatments, like the arthritis drug rituximab or intravenous immunoglobulin (IVIG), which is used to treat antibody deficiencies. The UCSF group said it’s also possible to create a “designer antibody” to deal with the problem.
A therapy to prevent severe viral disease could provide a stopgap measure to offset the dire need for vaccines in the current pandemic, and it would dramatically change the calculus of how society responds to future emerging viral threats.
“If we knew we had drugs to keep severe conditions from occurring – if the worst was in fact a lowly, one-week flu-like experience – imagine how different the world would be today,” Krummel said.
Authors: Other authors of the study include Alexis Combes and Arjun Arkal Rao, both of UCSF. The study was facilitated by a novel collaborative infrastructure developed by the Bakar ImmunoX Initiative at UCSF. Called CoLabs, this data and expertise-sharing infrastructure was key to this study, which mobilized dozens of participants across many clinical and basic science programs.
Funding: This work was supported by funds from the Bakar UCSF ImmunoX Initiative and funds from the NIH (R01 AI52116-S1, 3U19AI077439-13S1, NHLBI R35 HL140026); the American Cancer Society Postdoctoral Fellowship (#133078-PF-19-222- 01-LIB); and the Cancer Research Institute (Award # CRI2940). This project also has been made possible in part by grant number 2019-202665 from the Chan Zuckerberg Foundation.