Researchers at Washington University School of Medicine in St. Louis have conducted a study in mice to understand how prostate cancer cells respond to anti-hormone therapy by producing their own testosterone to fuel tumor growth. The research also suggests a potential drug combination that could inhibit the cancer cells from sustaining their growth.
In normal circumstances, healthy prostate cells do not generate testosterone. Therefore, this study provides valuable insights into how prostate cancer cells adapt to therapy that reduces testosterone levels, a common treatment option. The research reveals that aggressive prostate tumors can be slowed down in mice by inhibiting certain aspects of the hormonal fuel supply chain. This finding suggests a new approach to treating prostate cancer that has become resistant to the commonly used anti-testosterone therapy, abiraterone.
The study, published in the journal Nature Communications on June 9, may also contribute to understanding why Black men face a higher risk of developing prostate cancer and often experience more aggressive forms of the disease compared to white men of European ancestry.
Senior author Nupam Mahajan, PhD, a professor of surgery in the Division of Urologic Surgery, explains that while it is well-known that male hormones, specifically androgens like testosterone, drive the growth of prostate tumors, existing drugs that inhibit testosterone production eventually lose effectiveness. After approximately one year, androgen levels rise again, raising questions about the source of this androgen. The researchers discovered that prostate cancer cells adapt by increasing cholesterol production, which they convert into their own androgen. This study unveils a potential drug combination that could halt prostate cancer from sustaining its growth by targeting this mechanism.
In addition to his role at Washington University School of Medicine, Mahajan is also a research member of the Siteman Cancer Center at Barnes-Jewish Hospital.
The study delves into how prostate cancer cells detect a drop in androgen levels. The researchers identified a key protein called SREBF1, which acts as an androgen sensor when bound to the androgen receptor. When androgen levels decrease, this protein enters the nucleus of the cancer cell and recruits an enzyme called GCN5 to modify histone proteins through a process called acetylation. This modification activates various genes that are crucial for cholesterol and lipid production. Consequently, the cells produce substantial amounts of cholesterol, a necessary precursor for testosterone.
Mahajan explains that the cancer cells essentially overload the prostate with cholesterol and utilize it to generate more testosterone. This overload makes conventional pathways for testosterone production from cholesterol ineffective, rendering drugs like abiraterone ineffective as well.
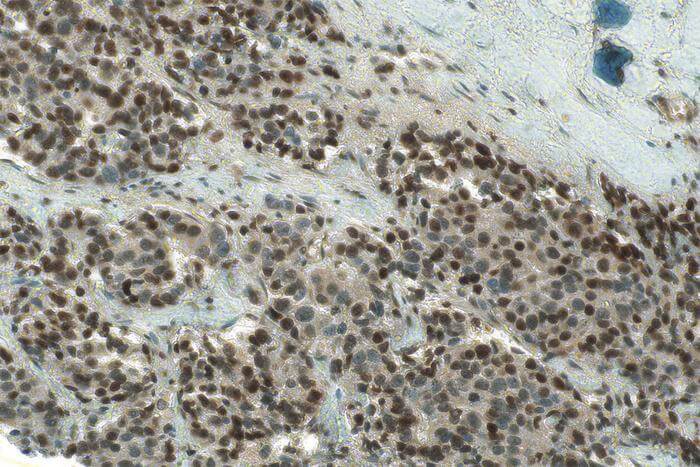
To validate their findings, Mahajan and his colleagues experimented with two inhibitors that target the molecular events responsible for excessive cholesterol production. They administered these inhibitors to mice with prostate tumors derived from human patients.
The first drug, afatinib, is an EGFR inhibitor approved by the FDA for certain types of lung cancer. The second drug is a GCN5 inhibitor, a class of drugs still under investigation in clinical trials. Mahajan notes that there is significant interest in developing GCN5 inhibitors due to their potential impact on gene regulation, cell growth, and inflammation. Mice treated with a combination of these two inhibitors exhibited significant reductions in tumor volume compared to those treated with a placebo or the anti-testosterone drug abiraterone alone.
The study also suggests that the abundance of cholesterol in aggressive prostate cancer could contribute to the racial disparities observed in this type of tumor. The researchers found evidence that the lipid profile of prostate cancer in African American men resembles the profile of treatment-resistant prostate cancer identified in the study. In other words, African American men with prostate cancer may have a greater tendency to exhibit an excess of cholesterol in their tumors compared to white men with the same tumor type, although the reasons for this remain unclear.
Mahajan emphasizes that this is preliminary data and requires further verification through larger studies. However,
the study suggests that the cholesterol profile may play a significant role in African American patients with prostate cancer. Given that African American men face a higher risk of prostate cancer and are diagnosed at earlier ages, understanding the link between their cancers and cholesterol production pathways could be crucial, particularly before commencing anti-testosterone treatment.
Mahajan expresses hope that the study will provide a strong rationale for conducting clinical trials with the combined inhibitors, targeting the cholesterol pathway, in patients with treatment-resistant prostate cancer.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!