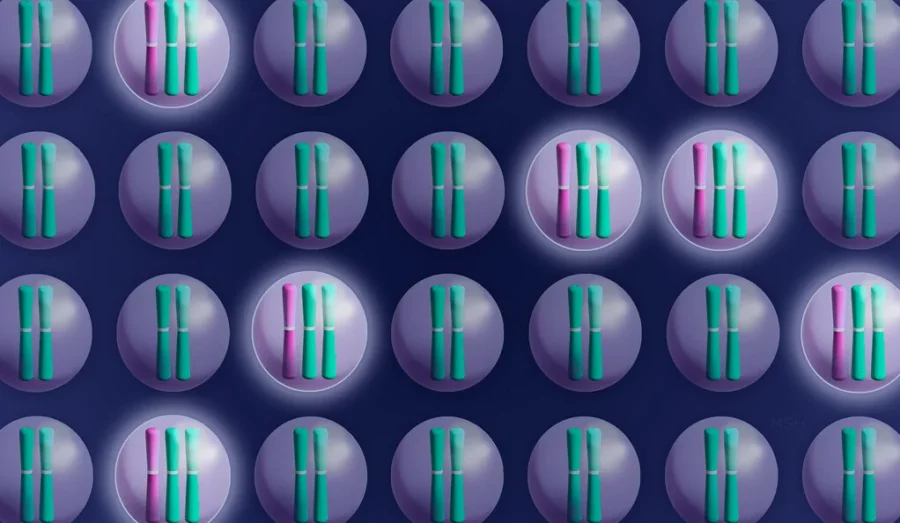
A groundbreaking study conducted by researchers at Yale University has revealed a significant breakthrough in cancer treatment. The study, published in the prestigious journal Science, highlights that cancer cells with additional chromosomes rely on these extra genetic components for their growth. By eliminating these chromosomes, the researchers were able to prevent the formation of tumors, pointing to a potential new avenue for treating cancer.
The lead author of the study, Jason Sheltzer, an assistant professor of surgery at Yale School of Medicine, emphasized the importance of this discovery. He explained, “If you look at normal skin or normal lung tissue, for example, 99.9% of the cells will have the right number of chromosomes. But we’ve known for over 100 years that nearly all cancers are aneuploid” – a condition characterized by an abnormal number of chromosomes.
Until now, the role of extra chromosomes in cancer development remained unclear, leaving researchers uncertain about whether they cause cancer or are a consequence of it. Sheltzer highlighted the challenge they faced: “For a long time, we could observe aneuploidy but not manipulate it. We just didn’t have the right tools.” However, using the gene-editing technique CRISPR, the team developed a novel approach to eliminate entire chromosomes from cancer cells. This breakthrough allows for a greater understanding of how aneuploid chromosomes function.
The study, co-led by former lab members Vishruth Girish and Asad Lakhani, targeted aneuploidy in melanoma, gastric cancer, and ovarian cell lines using their newly developed technique, called Restoring Disomy in Aneuploid cells using CRISPR Targeting (ReDACT). Specifically, they focused on removing an aberrant third copy of the long portion of chromosome 1, known as the “q arm,” which is frequently observed in various types of cancer and plays a role in disease progression.
Sheltzer revealed the outcome of their experiment, stating, “When we eliminated aneuploidy from the genomes of these cancer cells, it compromised the malignant potential of those cells, and they lost their ability to form tumors.”
Based on these findings, the researchers proposed the existence of an “aneuploidy addiction” in cancer cells. This term draws on previous research that demonstrated eliminating oncogenes, which contribute to the transformation of normal cells into cancer cells, disrupts the tumor-forming abilities of cancers. This concept led to the development of the “oncogene addiction” model of cancer growth.
Further investigations into the role of the additional copy of chromosome 1q in promoting cancer growth revealed that multiple genes were responsible for stimulating the proliferation of cancer cells when overrepresented due to being encoded on three chromosomes instead of the typical two.
The overexpression of these specific genes presented a potential vulnerability that could be targeted to treat cancers with aneuploidy. The researchers discovered that a gene encoded on chromosome 1, known as UCK2, was essential for activating certain drugs. Cells with an extra copy of chromosome 1 exhibited increased sensitivity to these drugs compared to cells with the typical chromosome count due to the overexpression of UCK2.
Furthermore, the study found that this heightened sensitivity allowed the drugs to redirect cellular evolution away from aneuploidy, leading to a cell population with normal chromosome numbers and a reduced potential to become cancerous. By exposing a mixture of 20% aneuploid cells and 80% normal cells to one of the UCK2-dependent drugs, the aneuploid cells decreased to just 4% of the mixture after nine days, in contrast to the 75% observed without drug intervention.
Sheltzer underscored the significance of these results: “This told us that aneuploidy can potentially function as a therapeutic target for cancer. Almost all cancers are aneuploid, so if you have some way of selectively targeting those aneuploid cells, that could, theoretically, be a good way to target cancer while having minimal effect on normal, non-cancerous tissue.”
Despite the promising implications, further research is required before this approach can be tested in clinical trials. Sheltzer and his team plan to advance their work by conducting studies on animal models, evaluating additional drugs and other aneuploidies, and collaborating with pharmaceutical companies to move closer to clinical trials.
Sheltzer expressed his team’s enthusiasm for clinical translation, stating, “We’re very interested in clinical translation, so we’re thinking about how to expand our discoveries in a therapeutic direction.” With continued progress, this pioneering research could pave the way for more effective and targeted cancer treatments in the future.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!