Novel Printing Technique Yields Artificial Veins Mimicking Human Tissue
Researchers at the University of Edinburgh have developed a new method to create artificial blood vessels using 3D printing technology. These gel-like tubes closely mimic the properties of human veins and could revolutionize heart bypass surgery, potentially improving outcomes for thousands of patients each year.
The innovative technique produces strong, flexible vessels that could replace both human and synthetic veins currently used in bypass operations. This advancement addresses longstanding challenges in cardiovascular treatment, offering a promising alternative that may reduce complications and improve patient recovery.
A Two-Step Process for Superior Artificial Vessels
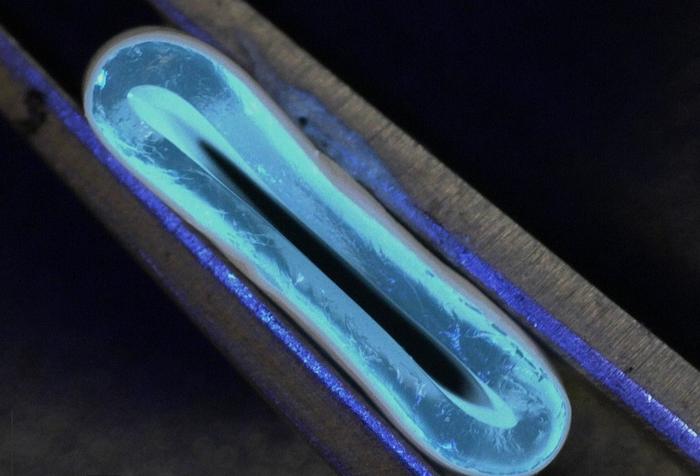
The research team, led by the University of Edinburgh’s School of Engineering, employed a two-stage process to create these artificial blood vessels. First, they used a 3D printer equipped with a rotating spindle to produce tubular grafts from a water-based gel. Then, they reinforced these grafts through electrospinning, a technique that uses high voltage to create a coating of ultra-thin nanofibers made from biodegradable polyester molecules.
Dr. Faraz Fazal, lead author of the study, explains the significance of this approach: “Our hybrid technique opens up new and exciting possibilities for the fabrication of tubular constructs in tissue engineering.”
The resulting artificial vessels demonstrated strength comparable to natural blood vessels. Moreover, their flexibility suggests they could integrate seamlessly into the human body. The researchers can produce these grafts in a wide range of sizes, from 1 to 40 mm in diameter, making them suitable for various applications in vascular surgery.
Dr. Norbert Radacsi, principal investigator of the study, highlights the potential impact: “The results from our research address a long-standing challenge in the field of vascular tissue engineering – to produce a conduit that has similar biomechanical properties to that of human veins.”
Why it matters: Heart bypass surgery is a common procedure, with approximately 20,000 operations performed annually in England alone. Current methods often involve harvesting veins from the patient’s own body, which can lead to scarring, pain, and increased infection risk. Alternatively, small synthetic grafts are used but can be challenging to integrate into the body and prone to failure.
The development of these 3D-printed blood vessels could significantly reduce these complications. By providing a readily available, customizable alternative to harvested veins, this technology could minimize the need for additional surgical sites on a patient’s body. Furthermore, the improved integration potential of these artificial vessels could lead to better long-term outcomes for bypass patients.
This research also opens up new possibilities in the broader field of tissue engineering. The ability to create complex, biomimetic structures through 3D printing and electrospinning could pave the way for advancements in other areas of regenerative medicine.
However, it’s important to note that this technology is still in its early stages. The next phase of research will involve testing these artificial blood vessels in animal models at the University of Edinburgh’s Roslin Institute. If successful, human trials would follow. This process ensures the safety and efficacy of the new vessels before they can be widely used in clinical settings.
As cardiovascular disease remains a leading cause of death worldwide, innovations like this could have far-reaching implications for global health. The ability to produce artificial blood vessels that closely mimic natural ones could not only improve surgical outcomes but also potentially reduce healthcare costs and increase accessibility to life-saving procedures.
Looking ahead, this research opens up exciting possibilities for personalized medicine in cardiovascular care. Future developments might include the ability to tailor artificial blood vessels to individual patient needs, further improving surgical outcomes and patient quality of life.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!