Low birth weight infants are host to numerous microorganisms immediately after birth, and the microbiomes of their mouths and gut start out very similar but differentiate significantly by day 15 according to a study published in mBio®, the online open-access journal of the American Society for Microbiology.
“We could watch this differentiation over time. With each passing day, two body sites [mouth and distal gut] became more and more differentiated from each other. It was a consistent pattern,” says co-author Elizabeth K. Costello of Stanford University.
Low birth weight infants, who are often born premature, are more susceptible than normal weight infants to invasive infections like necrotizing enterocolitis, a vulnerability that may be related to colonization by bacteria from their surroundings. Unlike adults, the microbiomes of the mouth, skin, and gut of infants right after birth are undifferentiated, says Costello – the microbiomes look more or less similar at each of these body sites. The researchers sought to find out how rapidly the communities of microbes in these different sites take on a character of their own.
They examined changes in the oral, skin, and gut microbiomes of low birth weight infants over the course of the first three weeks after birth and found that although the microbiomes in each of these sites start our markedly similar, they gradually differentiate over time. This is the first time the differentiation of the microbiota in multiple body sites in newborn infants has been investigated.
“We chose to look at premature infants between the ages of eight and 21 days old and asked, over this time period, what is going on with their oral, gut and skin communities,” says Costello. The period from 8 to 21 days after birth marks a critical window for colonization of an infant, and it’s also the period of onset for necrotizing enterocolitis (although none of the infants in this study were struck by the disease).
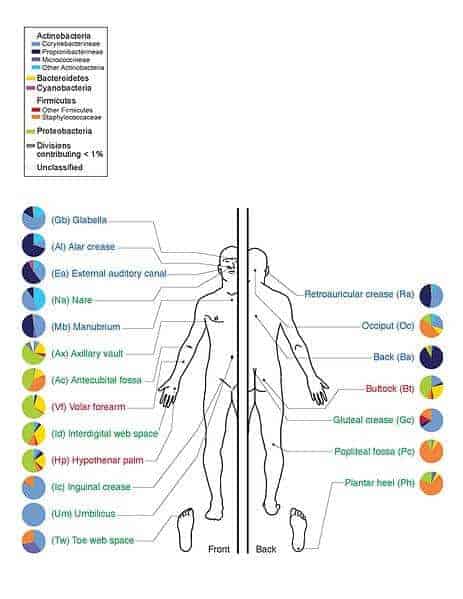
The researchers collected stool, saliva, and skin swabs from six low birth weight infants (five of whom were born premature) that ranged in weight from 1.65 – 4.01 lbs on postnatal days 8, 10, 12, 15, 18, and 21. They amplified, pyrosequenced, and analyzed the bacterial 16S genes present in each sample and compared them with analogous data from normal-birthweight (NBW) infants and healthy adults.
In the 8 – 21 day age range, there was a subtle but important divergence in the composition of the oral and gut microbiotas, a differentiation that was mostly driven by changes that evolved in the composition of the gut microbiome. The babies’ microbiomes were also dominated at times by bacterial types that have been associated with newborn infections and necrotizing enterocolitis, including Staphylococcus, C. perfringens, P. aeruginosa and others.
The scientists also tracked the effects of antibiotic treatment in one infant in the study, noting the rise of a type of Mycoplasma in the mouth that has previously been associated with vaginal infection.
Of the three sites studied, neonatal skin was the most adult-like in its microbiota composition. And like healthy adults, the microbiota of the different body sites in the infants was apparently determined mostly by body site and by host individual.
Co-author Michael J. Morowitz of the University of Pittsburgh School of Medicine says understanding the vulnerability of preemies from a microbial perspective can provide insights into how to better care for them.
“Premature infants are unique because they can spend several months in the hospital, where they’re exposed to virulent bacteria, they also frequently have antibiotics exposure, and they’re dietary intake is irregular – sometimes they’re not able to eat anything by mouth. That probably effects colonization patterns,” says Morowitz. “The first step [in understanding this] is to define what’s normal for these infants and what’s abnormal.”
Morowitz, Costello and others are currently working on a larger study to expand on these results. By studying more babies, and by monitoring microbial colonization of low birth weight infants who eventually develop infections like necrotizing enterocolitis, they hope to better pinpoint the microbial profile of babies who are susceptible to disease, hopefully leading to more informative surveillance techniques and better interventions to help keep these most vulnerable infants on the path to becoming healthy children and adults.