Duke University researchers have developed a promising new pain reliever that works through an entirely different mechanism than opioids, potentially offering millions of chronic pain sufferers an alternative without the dangerous side effects of addiction and tolerance. The experimental drug, called SBI-810, targets specific receptors on nerves and in the spinal cord while avoiding the brain’s reward pathways that make opioids so problematic.
The findings, published May 19 in Cell, demonstrate that SBI-810 effectively treats both acute pain—like that from surgery or injury—and chronic pain from nerve damage in animal models. What makes this compound particularly exciting is its precision: rather than flooding the body with broad chemical signals like traditional painkillers, SBI-810 activates only specific cellular pathways linked to pain relief.
As the U.S. continues to grapple with an opioid crisis claiming more than 80,000 lives annually while one-third of Americans suffer from chronic pain, the need for safer, effective alternatives has never been more urgent. Could this targeted approach finally break the cycle of addiction and ineffective treatment that has plagued pain management for decades?
A Smarter Approach to Pain Relief
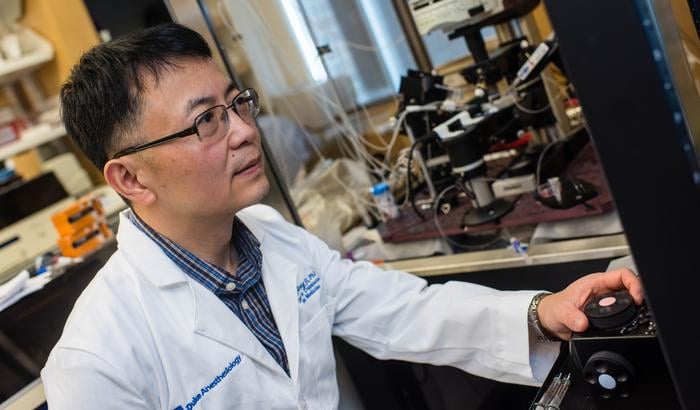
“What makes this compound exciting is that it is both analgesic and non-opioid,” said senior study author Ru-Rong Ji, PhD, an anesthesiology and neurobiology researcher who directs the Duke Anesthesiology Center for Translational Pain Medicine.
Unlike opioids, which indiscriminately activate multiple cellular pathways throughout the body and brain, SBI-810 targets a specific receptor called neurotensin receptor 1 (NTSR1). This receptor is found on sensory neurons and throughout the central nervous system, making it an ideal target for pain management.
The drug uses a sophisticated method called “biased agonism” to activate only a specific cellular signal—β-arrestin-2—linked to pain relief, while avoiding other signals that can lead to side effects or addiction.
“The receptor is expressed on sensory neurons and the brain and spinal cord,” Ji explained. “It’s a promising target for treating acute and chronic pain.”
Powerful Results Across Multiple Pain Types
In laboratory tests, SBI-810 demonstrated remarkable versatility and effectiveness in treating different kinds of pain:
- Relieved pain from surgical incisions, bone fractures, and nerve injuries
- Reduced signs of spontaneous discomfort, including protective behaviors and facial grimacing
- Outperformed gabapentin, a common medication for nerve pain
- Showed better results than oliceridine, a newer hospital-grade opioid, in some pain models
- Maintained effectiveness with repeated use, avoiding the tolerance problem that plagues opioid treatment
Perhaps most significantly, the compound didn’t cause memory problems or sedation, which are common side effects of gabapentin and similar drugs prescribed for chronic pain.
How It Works: Targeting Pain at Its Source
SBI-810 works through multiple mechanisms in both the peripheral nervous system (nerves throughout the body) and the central nervous system (brain and spinal cord). In the spinal cord, the drug reduces the transmission of pain signals between neurons, effectively dampening the pain message before it reaches the brain.
In sensory neurons, SBI-810 suppresses the electrical firing that signals pain and reduces the expression of Nav1.7, a key protein involved in transmitting pain signals. This dual action allows the drug to block pain at multiple points in the nervous system.
Crucially, when tested alongside opioids, SBI-810 made them more effective at lower doses—potentially allowing for reduced opioid use while maintaining pain control. It also prevented common opioid side effects like constipation and reduced withdrawal symptoms, which contribute to addiction.
From Lab to Patients
Though still in early development, Duke researchers are aiming to begin human trials soon. The university has secured multiple patents for the discovery, signaling confidence in its potential as a marketable treatment.
The research team envisions SBI-810 as a treatment option for various pain scenarios, from post-surgical recovery to chronic conditions like diabetic nerve pain and lower back pain.
The study’s findings align with broader efforts to address America’s dual crises of pain management and opioid addiction. While drug overdose deaths have begun to decline, the massive number of Americans suffering from chronic pain—and the limited effective treatments available—remains a pressing public health challenge.
If human trials confirm the promising results seen in animal studies, SBI-810 could represent a significant breakthrough in pain medicine: a treatment powerful enough to relieve serious pain yet precise enough to avoid the devastating side effects that have made opioids so problematic.
For the millions of Americans caught between untreated pain and the risks of current medications, this new approach offers a glimpse of what pain management might look like in the future—effective relief without the high, addiction, or diminishing returns that have defined pain treatment for generations.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!