A new pilot study by Carnegie Mellon University researchers investigates the mechanisms that underlie a treatment for patients with amblyopia, also known as “lazy eye.”
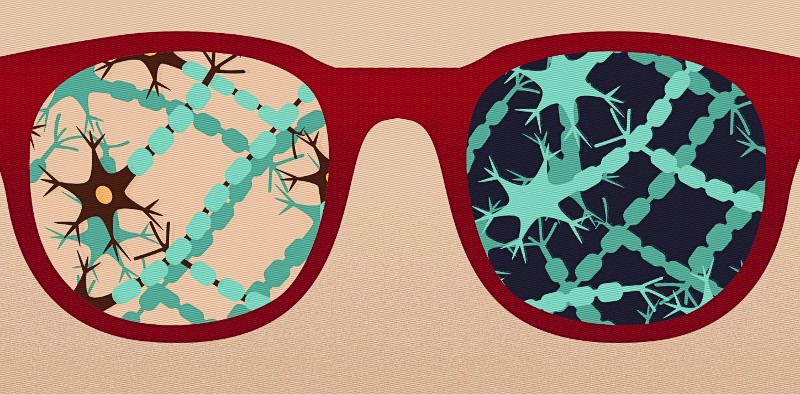
Amblyopia is a condition where the brain cannot recognize sight from one eye and favors the other eye. One therapy that shows promise for addressing the condition in adult patients is transient dark exposure, in which a patient has an occlusion that caused their amblyopia removed and lives in darkness for a few days.
The study by researchers in Carnegie Mellon’s Mellon College of Science and the College of Engineering found evidence that a week after transient dark exposure, the brain’s neural networks adjust the way they process visual information thereby improving vision. The findings were published in eLife.
“One of the big things in neuroscience is to try to understand how we have stable perception,” said Sandra Kuhlman, assistant professor of biological sciences at Carnegie Mellon and the head of the Kuhlman Lab. “The field is now able to identify adaptive properties of neural circuits on long time scales. That’s really important to understand how neural function underlies basic sensory processes.”
Brian Jeon, a postdoctoral fellow and graduate of Carnegie Mellon’s Department of Biological Sciences, conceived the study as a Ph.D. student working in Kuhlman’s lab.
“Transient dark exposure is a treatment that people are exploring in humans,” Jeon said. “We said, ‘hey, maybe this has to do with how the brain encodes information, and maybe that gets disrupted when you remove inputs for an extended period of time.’ We found there is some room for change, but actually, the system is very resilient.”
The researchers use two-photon calcium imaging to record neural activity in adult mice before and after transient dark exposure. This technique allows scientists to measure entire networks of neurons in living models.
At the beginning of the study, mice were presented with visual stimuli, and their neural responses were recorded. After darkness exposure for eight days, the same stimuli were presented again to the mice and their visual responses were also recorded.
“Brian’s data helps shed light on the various, complex factors that drive plasticity in the visual cortex, and bring us one step closer to understanding how eye injury and disease might affect visual perception,” said Steven Chase, professor of biomedical engineering and a co-author on the paper.
Though the mice exhibited some issues with visual processing within a few days after exposure, they recovered after a week.
The researchers aim to use the study’s techniques for a longer-term study or one with younger mice. They also want to apply the technique of two-photon calcium imaging when modeling and studying other neurological and psychiatric conditions.
“There’s so many things we don’t understand at a cell type specific level in neural circuits,” Kuhlman said. “We hope that the analytical approach will be useful for other researchers.”
Jeon, Chase and Kuhlman were joined by Biological Sciences Researcher Thomas Fuchs on the project “Visual Experience Has Opposing Influences on the Quality of Stimulus Representation in Adult Primary Visual Cortex.” The project received funding from the National Institutes of Health’s National Eye Institute and the Curci Foundation.