New Technology Could Expand Access to Crucial Heart Diagnostics
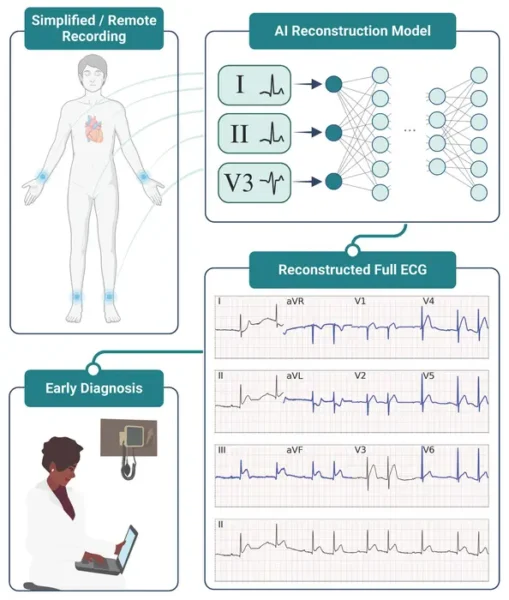
Researchers at Scripps Research have developed an artificial intelligence (AI) tool that can accurately diagnose heart conditions using data from just three electrocardiogram (ECG) leads, instead of the standard 12. This innovation, published in npj Digital Medicine on August 1, 2024, could make heart monitoring more accessible and affordable without compromising accuracy.
The AI algorithm can recreate a full 12-lead ECG from data collected by only three leads. When cardiologists reviewed these AI-generated ECGs, they could identify heart attacks with nearly the same accuracy as when reviewing traditional 12-lead ECGs.
Bridging the Gap in Heart Diagnostics
Standard 12-lead ECGs require specialized equipment and expertise, which aren’t available in all healthcare settings. This new approach could bring high-quality heart diagnostics to more patients, potentially saving lives through earlier detection of heart problems.
Dr. Evan Muse, lead of cardiovascular genomics at Scripps Research Translational Institute, explains the significance: “This opens up the door to patients being able to get really high-quality, time-sensitive clinical data without traveling to somewhere that has a 12-lead ECG. It likely means not only increased access to ECG technology, but decreased costs and improved patient safety.”
Why it matters: Heart disease remains a leading cause of death worldwide. Timely and accurate diagnosis is crucial for effective treatment. By simplifying the ECG process without sacrificing accuracy, this AI tool could help more people get the cardiac care they need, especially in underserved or remote areas.
The research team, led by Dr. Giorgio Quer and Dr. Evan Muse, used over 600,000 12-lead ECGs to train their AI algorithm. Half of these ECGs showed normal heart rhythms, while the rest displayed various heart conditions. This diverse dataset helped ensure the AI could handle a wide range of cardiac scenarios.
To test the AI’s performance, the researchers presented 238 ECGs to cardiologists, with half showing signs of a heart attack. The doctors reviewed either the original 12-lead ECG or the AI-reconstructed version from three leads. Remarkably, the cardiologists couldn’t tell which was which, and their accuracy in identifying heart attacks was nearly identical: 81.4% for AI-generated ECGs versus 84.6% for original 12-lead ECGs.
This level of accuracy is crucial for real-world applications. Dr. Quer emphasized, “It was important to us that we not only show that this algorithm works at a technical level, but that the data generated by the algorithm can be accurately interpreted by cardiologists.”
While these results are promising, the researchers caution that more studies are needed before the tool can be used for clinical decision-making. Future research will test the algorithm with different patient populations and in various clinical settings to ensure its reliability across diverse scenarios.
Dr. Eric Topol, director of the Scripps Research Translational Institute, highlighted the broader implications: “This is an optimal case for AI—taking a few leads of the (12-lead) electrocardiogram—to make it remarkably informative, which has big practical implications for patients in the future.”
This research is part of a growing trend in using AI to enhance cardiac care. In 2023, the same group showed that a single ECG patch worn for two weeks could help predict atrial fibrillation risk, demonstrating the potential of AI in long-term heart monitoring.
Looking ahead, this technology could pave the way for more accessible heart diagnostics in various settings, from rural clinics to home care. As AI continues to evolve, we may see even more innovative applications that expand the reach and effectiveness of cardiac care, potentially saving countless lives through earlier and more accurate diagnoses.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!